So I have my blood results after 6 weeks on 10mcg T3 trial (5 mcg x 2 daily) as well as 75mcg of Levo and I know my endo (NHS) will phone this week and I want to be well prepared.
10/8/22
TSH 0.06 (0.35-5)
T4 12.2 (9-21) 27% through range
T3 4.8 (3-6) 60% through range
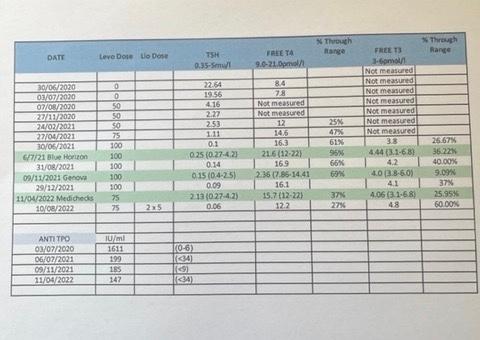
Previous results, pre T3, are shown in the photo attached. Green highlights show private test results and the others are NHS tests.
I am feeling the best I’ve felt in a long time - more energy, much more sleep and less brain fog (though this could still improve). I still have other symptoms but probably liveable with for the moment. My concern is the suppressed TSH and low T4. The endo said he wanted to see my TSH around 2 (help!) so isn’t going to be happy with these figures.
Any suggestions as to how things might be adjusted? Or suggestions for best way to deal with the suppressed TSH and low T4 when the endo phones?
Thank you for all your help and support.