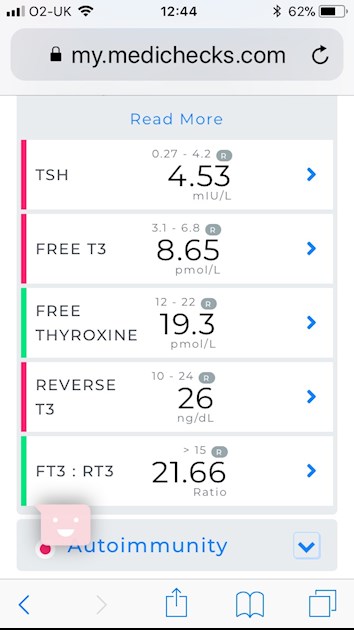
Still getting results like these.
Blood taken 9am, fasting. No t3 for 12 hours.
Currently on 50mcg levo and 20mcg t3
Folate 6.8 <3.5
Vitamin d 243 (50-175)
B12 300 (37-188)
Ferritin is 83 on this test but recent gp iron panels showed low ferritin (47) iron saturation at 20% (20-60) and so I believe iron is an issue for me. I know b12 and vit d is high as I am supplementing as I have a compromised immune system. Cortisol all ok except waking needs to be slightly higher I believe (previous post)
Anyone else scratch their brains at all for what I should do please?? I’m not well. Have been discharged by addembrookes as their tests showed tsh 2.5 and high t3 and they were fine with that....
Boshus i know you are overrange on t3- is this like you?
As I said I have a compromised immune system and have 2 co infections that my functional medicine doc has said might be blocking my thyroid receptors.
I’m working on raising iron. I know rt3 tells you there’s a problem but doesn’t pin point.
Had an mri and no issues there...
Main issue is debilitating fatigue, digestive issues, cold hands and feet, tremors (seen a neurologist- I believe this is the infections) aches. Blood pressure is always low normal and pulse around 68.
Gluten/ sugar/ dairy free/ grain free Organic diet etc etc!
Should i keep raising t3????
Thank you....
One plus is my antibodies have gone right down and only just over top of ranges to conform hashi.