Hi all
Had rai in oct 18
Since then I have had the following problems
Weight loss
Abdomen pain colon
Tired
Gluten and dairy free NOW
Caffeine problems
Mental health
Muscle loss
Doc thinks it’s
Any one else has this issue after RAI?
Hi all
Had rai in oct 18
Since then I have had the following problems
Weight loss
Abdomen pain colon
Tired
Gluten and dairy free NOW
Caffeine problems
Mental health
Muscle loss
Doc thinks it’s
Any one else has this issue after RAI?
What are your recent thyroid results, which replacement and what dose are you taking ? It's possibly you are reacting to the tablets you are on.
Hi
I take 150mcg activis
Can go any higher I lose my mind
We need to see thyroid blood results, TSH, T4 and T3 plus the ranges. You may need to try a different brand of Levo, finding the right treatment is trial and error.
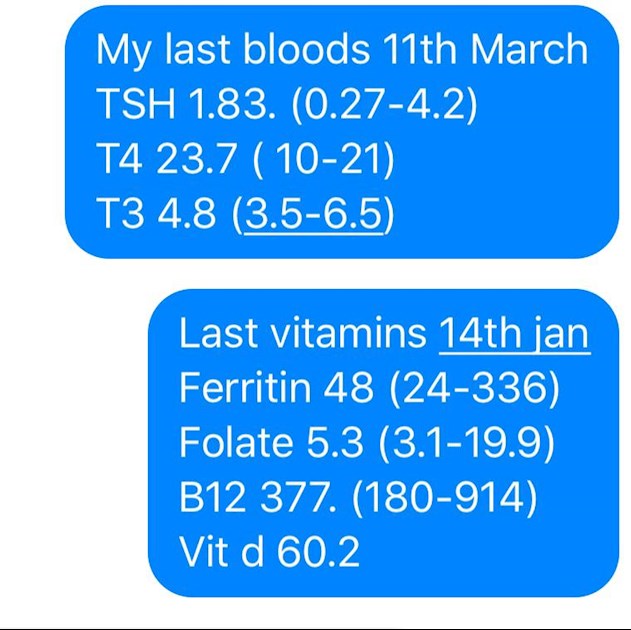
Thanks. I put a photo of my bloods on the 1st post for you
They show you aren't converting very well as T4 is over range yet T3 is very low in range plus your TSH is to high, you may need a combination of Levo plus T3 but getting that prescribed will be a challenge.
I have bought some T3 my self. Just worried I may lose the plot again and the anxiety may come back
Money is not a issue for me. Just don’t know enough
Roughly where in the UK are you?
You should see a knowledgeable thyroid specialist
Before starting on T3 ideally vitamin levels need to be optimal
New NHS England Liothyronine guidelines November 2018 clearly state on pages 8 & 12 that TSH should be between 0.4-1.5 when treated with just Levothyroxine
Note that it says test should be in morning BEFORE taking Levothyroxine
Also to test vitamin D, folate, B12 and ferritin
sps.nhs.uk/wp-content/uploa...
Do you always get same brand of Levothyroxine?
Always take Levo on empty stomach and then nothing apart from water for at least an hour after.
Many take Levothyroxine early morning, on waking, but it may be more convenient and possibly more effective taken at bedtime.
verywell.com/should-i-take-...
Other medication at least 2 hours away, some like HRT, iron, calcium, vitamin D or magnesium at least four hours away from Levothyroxine
Many people find Levothyroxine brands are not interchangeable.
Once you find a brand that suits you, best to make sure to only get that one at each prescription. Watch out for brand change when dose is increased or at repeat prescription.
Many patients do NOT get on well with Teva brand of Levothyroxine. Though it is the only one for lactose intolerant patients
North east England
Same brand activis
I have just found out I am intolerant to milk
Guess it was the rai
Should I take teva?
Teva is the only tablet for lactose intolerance
Try Teva brand first.
Get bloods retested 6-8 weeks after changing brand
If no good then there is liquid Levothyroxine, but they don't like to offer it as it's expensive
Lactose intolerance is common with thyroid issues
Getting vitamins optimal is essential
Which Dr has diagnosed you with that condition? If it's your GP or your Endo surgeon rather than a gastroenterologist, you need a referral to the latter for not only a firm diagnosis, but to identify the cause (there may be a direct correlation between the BAM and the RAI, or it might be a red herring and there could be another cause such as Crohn's or whatever) and for treatment to be initiated as necessary. Your vitamin & mineral results are low and your nutrition needs to be considered within the overall investigation of your absorption problems as clearly it can affect all aspects of your physical, psychological and thyroid health, as you are discovering.
Hi Maisie.
Had a colonoscopy so rules out crohns
It was a Gi specialist who said IBS
Don a seh scan and waiting results
Can I do anything to help my self at the mo?
Hi dodge1979 So glad you don't have Crohn's, my elder son does, and I'd not wish it on anybody. A 2015 study published in the Royal College of Medicine's journal 'Clinical Medicine' reported that more than 60% of IBS-D diagnoses were wrong, and that other organic diseases such as BAM, were missed. So if you had a scan, presumably your GI specialist is testing out his initial IBS diagnosis - was it a nuclear medicine SeHCAT scan where you had to swallow artificial bile acid in a capsule or drink? Good luck with the results.
As for what you can do at present, eating low fat may be a key requirement post-diagnosis; so you could start that now and see if it helps with symptoms (< 40 g per day). Ensuring other than that, that you are getting optimal nutrition in your diet, so that whatever you manage to absorb from it, is good quality; and sublingual vitamin supplements that are absorbed directly to the blood stream avoiding the GI tract, may be helpful. But if it were me, I'd take your Consultant's advice, and especially that of the dietician/nutritionist, if you are referred to one. In fact, if you do test positive for BAM, perhaps insist on a referral even if not offered to you.
When I read your post I thought 'what is bam'. I guess it means Irritable Bowel Syndrome!
We have members who've suffered as you are at present. It can be resolved, slowly, slowly.
You have been given levothyroxine, which is T4 only. My personal opinion, and I have a thyroid gland, is that those who do not should be given a combination of T4/T3 (levothyroxine/liothyronine). Researchers have stated that a combination dose of 4:1 or 3:1 is beneficial.
Welcome to our forum and I'm very sorry you feel awful. I have hypothyroidism so you also have had RAI to knock out your gland altogether so you have my sympathies.
Members who've had RAI will respond when they read your post.
First of all I shall give you some hints for your next blood test.
All blood tests have to be at the earliest possible, fasting (you can drink water) and allow a gap of 24 hours between last dose of levo and test and take afterwards.
Take thyroid hormones with one full glass of water and wait an hour before eating. Some prefer a bedtime dose, in that case you should last eat about 3 hours previously.
I have my thyroid gland but could not recover on levothyroxine at all - though many do - but am well on liothyronine. Unfortunately in the UK they have withdrawn this life-giving hormone due to the cost of it. The suppliers increased their price astronomically that NHS cannot afford it.
Blood tests have to have the ranges stated. Labs differ in their machines and therefore ranges can be different and ranges are need for members to respond.
Other members will respond re your other blood test results.
It is a big learning curve but we can recover our health, despite what the doctors state as their hands are now tied.
Levothyroxine is an inactive hormone. It has to convert to T3.
T3 is the Active thyroid hormone and it is need in the millions of T3 receptor cells - brain and heart contain the most.
If you're in the UK, we used to have 'options' prescribed which is NDT (natural dessicated thyroid hormones made from pigs' thyroid glands and contains all of the hormones a healthy gland would do, i.e. T3, T4, T2, T1 and caclitonin.) We also used to get T3 added to T4 or T3 alone. T3 was withdrawn a few months ago due to exorbitant cost going up 6,000% a wonderful opportunity for those medical professionals who wanted levothyroxine to be the only option for us. I for one cannot abide levo. I am well on T3 but that's not to say everyone will. Many of us need to find out, gradually, what suits us.
Millions appear to be well on levothyroxine alone. Many doctors are fixated with the TSH and if it is low assume we've gone hyPERthyroid and adjust dose up/down to 'fit it into a range'. The aim really should be to make the patient well again. Also vitamins/minerals have to be optimum too.
BAM is a distinct chronic disease in its own right, which is often misdiagnosed as IBS.
Thank you MaisieGray for enlightening me upon this and if it is chronic disease all the more care should be taken by the doctors for the patients. I don't understand why the professionals cannot fathom out why the person in front of them is struggling and are looking to them for advice/care.
I think IBS is an easy catch-all when we have gut pain/constipation/diarrhea isn't it (although when I first took my then baby son to the GP, his symptoms were put down to me being an over-anxious mother ....) despite apparently more than 60% of IBS-diarrhea predominating cases being wrongly diagnosed as such. The study I'm quoting concluded "BAM is a cause for GI symptoms in around half a million people who are currently being treated for IBS-D in the NHS" so money is being wasted on the wrong investigations and treatments, and people aren't getting better; whereas "This study has demonstrated that the use of low-fat dietary interventions in patients with a SeHCAT scan result <20% leads to clinically important improvement in GI symptoms and should be widely used."
All vitamin levels are too low. This is likely due to inadequate thyroid replacement. Either you need higher dose of Levothyroxine or (because FT4 is already high) the addition of small dose of T3
Recommended on here that all thyroid blood tests should ideally be done as early as possible in morning and fasting. Last Levothyroxine dose should be 24 hours prior to test, (taking delayed dose immediately after blood draw). This gives highest TSH, lowest FT4 and most consistent results.
Is this how you did the test?
Getting vitamins optimal is first step. Then conversion may improve
Vitamin D is too low. GP will only prescribe to bring vitamin D up to 50nmol. So you will need to improve by self supplementing to at least 80nmol and around 100nmol may be better .
Once you Improve level, very likely you will need on going maintenance dose to keep it there.
Retesting twice yearly via vitamindtest.org.uk
Vitamin D mouth spray by Better You is good as avoids poor gut function.
It's trial and error what dose each person needs. Frequently with thyroid disease we need higher dose than average
Local CCG guidelines
clinox.info/clinical-suppor...
Government recommends everyone supplement October to April
gov.uk/government/news/phe-...
Also read up on importance of magnesium and vitamin K2 Mk7 supplements when taking vitamin D
betterbones.com/bone-nutrit...
articles.mercola.com/sites/...
healthy-holistic-living.com...
sciencedaily.com/releases/2...
articles.mercola.com/sites/...
betterbones.com/bone-nutrit...
This article explains should discuss with specialists before taking any vitamin K if you take any blood thinning medication
drsinatra.com/vitamin-k2-su...
B12 and folate on the low side.
Supplementing a good quality daily vitamin B complex, one with folate in not folic acid may be beneficial.
chriskresser.com/folate-vs-...
B vitamins best taken in the morning after breakfast
Recommended brands on here are Igennus Super B complex. (Often only need one tablet per day, not two. Certainly only start with one tablet per day after breakfast. Retesting levels in 6-8 weeks ).
Or Jarrow B-right is popular choice, but is large capsule
If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 7 days before any blood tests, as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
Ferritin too low, needs to be at least half way in range. Eating liver or liver pate once a week plus daily vitamin C may help improve absorption of iron. Other iron rich foods like spinach, pumpkin seeds, dark chocolate
Selenium supplements can help improve conversion of FT4 to FT3
Only add one supplement at a time and wait at least ten days to assess any reaction before adding another