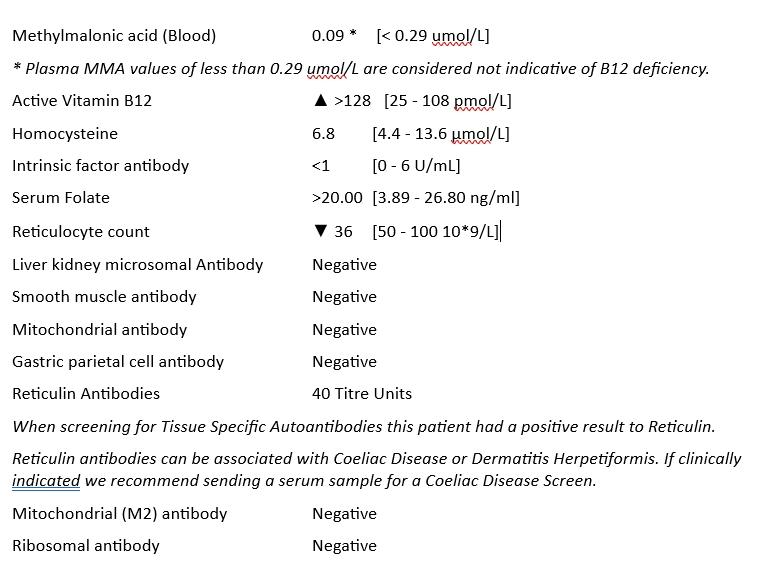
Hi Everyone. So here I am on my health journey with some results. These were the Blue Horizon Pernicious Anaemia Profile taken 4 weeks ago. I had no supplements at all for 6 weeks prior. I SI 0.7mg B12 Hydroxy 6 weeks before.
My plan, following very frustrating GP appointments has been to have the tests, then start a therapeutic trial of supplements to rule things out or in (either of these is progress I reckon!) while I await the results.
Since having the bloods, I've been SI B12 Hydroxy for 4 weeks every other day, along with supplementing 40mg gentle iron per day. I started on A-Z multivits around 4 days ago.
Many of my symptoms have lessened or disappeared in that time, including low mood, breathlessness, concentration, fatigue, tingling in feet, burning/numb/twitching face and burning hands.
So, the things I'd appreciate any help with are:
1. As far as I can see, these results indicate I don't have PA, or any issues with low B12. Is that correct?
2. They did flag the low reticulocyte count, but as my iron levels were OK, didn't comment further. They didn't test ferritin however, which my GP results show have been below 30 for some time. Again, I'd welcome any thoughts from anyone with more knowledge than me on this.
3. Also, a positive for Reticulin Andibodies. I believe this is indicative of coeliac or Crohn's disease? My previous coeliac tests have all been negative, although the GP tests do not give a range. I'm going to post on the Gluten Free Guerrilla's forum for more advice, as I frequently have tummy bloating.
4. The only other thing I keep finding is my folate levels are consistently high, despite my not supplementing. Again, any thoughts would be welcome.
So, I guess from my 'therapeutic trial' so far, at least something is working, although the cause of my issue is still uncertain. Again, any thoughts welcome - including that I can rule B12 out of the equation. 😊
Thanks in advance you lovely people! 😊