A recent post discussed the trial in China on the high dose protocol for Besremi. The discussion focused mostly on VAF (mutation) results. The other important item we can miss is CHR (blood response)
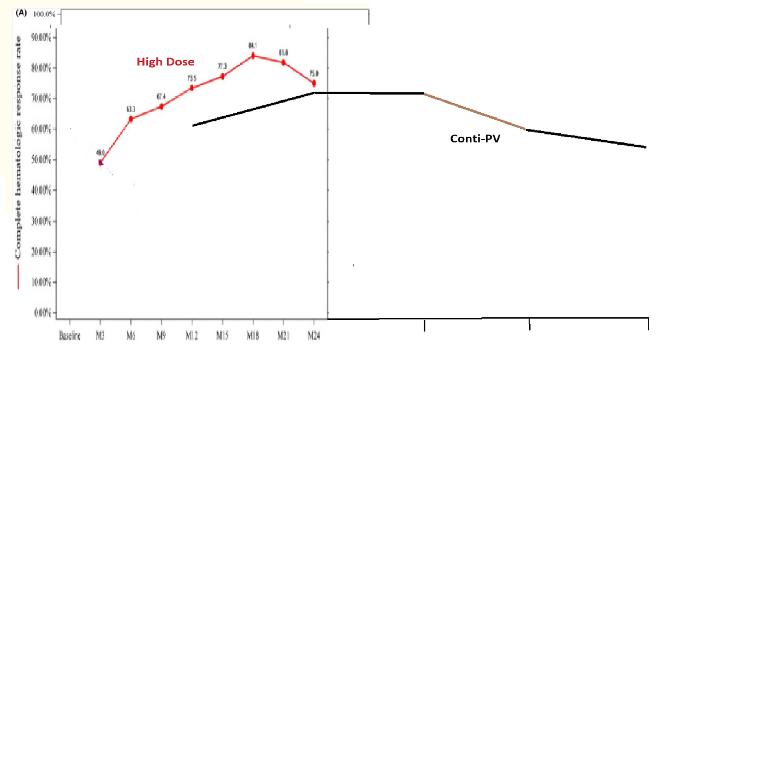
I made a plot comparing CHR vs Time from the Proud/Conti PV trial to the recent high dose trial. The ContiPV has a text table I used for this plot. Both trials used high maintenance doses, Conti PV being ~400mcg, but the Chinese trial started more aggressively.
Most trials of all 3 of our drug types report some loss of best CHR over time, these follow this trend. Assuming they are comparable, this plot suggests a possible faster best-CHR burn out with the high dose protocol. Maybe the Chinese trial will report a third year to get a better comparison.
One subtle item in the Chinese trial is the starting the premise that CHR and MR (molecular) have been assumed to be connected while this trial showed a disconnect. Some confirmation that this CHR-MR connection has been previously acknowledged, I've posted often on it. If the high dose method breaks the connection, is that desirable? Or is it instead just bringing all the effects forward?
A related question, if best-CHR burnout is faster, will VAF rise start sooner. Or will the rise be avoided/delayed? The median starts slightly rising after 5 years in the IFN trials where this was knowable.
--
(Chinese trial) pmc.ncbi.nlm.nih.gov/articl...
(Conti PV) mpn-hub.com/medical-informa...
(ContiPV doses, see bar plot) healthunlocked.com/mpnvoice...