I'm working on a discussion of CHR vs molecular response (MR or allele burden, AB) on INF. In a recent post I discussed CHR correlates to MR.
healthunlocked.com/mpnvoice...
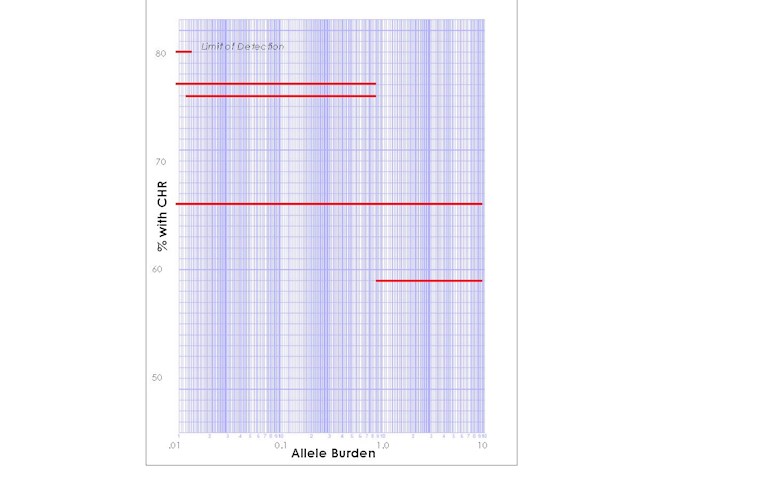
Here are results for the best of the reductions in the 5 year Bes trial.
The data here show that the best responses among the good ones also had the best rate of CHR, matching the pattern for the other reports above.
--
From Table 5 of the supplement to the 5 year Ropeg report I turned the text into this plot. (I had to think about Log plots, a college flashback)
The red lines are the ranges of AB after 5 years on Bes. Higher is better CHR, left is better MR.
The top left is no Jak2 detected (<0.014%). These started with 14-56%AB. 80% of these had CHR.
The lower right is still good response, 1-10% AB but not as good as the other sets here. It had the lowest CHR rate at 59% with starting AB of 10-84%.
So the pattern from before persists, having CHR on INF favors lower AB on INF. Also lower starting AB was favorable.
Plot using Table 5 from: