In a recent thread one report has HU providing a strong benefit to marrow, esp for ET, but some in PV too, discussed here:
healthunlocked.com/mpnvoice...
This is a surprise. So I did a quick search and two further reports come up supporting this idea.
Are we missing important info in our trade offs of benefits? The improvement is fast if it happens, 6-12 months, so finding out would not delay IFN start much if IFN is the ultimate plan. Is it durable? No info on that I can find.
If it's durable, might it be a good idea to start with HU even if IFN is the end goal? Many of us do this anyway. At least having BMBs before and after 1 year of HU seems indicated here.
But it's possible this marrow improvement is most obvious only at the 1st year. This would be similar to the ~ 1 year allele benefit seen with HU.
This all begs for more info.
Have any members had BMBs before and after a year of HU?
--
One report, 22 years ago:
pubmed.ncbi.nlm.nih.gov/106...
This is for myelofibrosis in context of CML, so not right on the point of MPN, but should be relevant. It likely used the early non-peg IFN so that would be a negative on the IFN side. But the result was clear at least for CML:
-"monotherapy by IFN exerts a fibrogenic effect" (promoting the development of fibers)
-"HU treatment seems to prevent and even resolves bone marrow fibrosis in CML"
-"changing content of reticulin fibres was usually accompanied by corresponding alterations in the number of CD61+ megakaryocytes" (megas are especially relevant to ET, maybe that's why the report at top has ET with the higher 50% benefit rate.
-Combo with IFN was less effective but also present: "To a lesser degree, these changes were also expressed in the cohort with a combined IFN and HU regimen."
-"Further evaluations revealed that these effects had occurred within the first year, mostly after 6 months of treatment"
--
A 2nd report:
cdn.mdedge.com/files/s3fs-p...
This is just a single patient in an informal report, but it's for actual MPN.
Background info in there:
-Anagrelide should not be 1st line therapy: "Many previous studies have linked anagrelide with progression of bone marrow fibrosis in patients with MPNs"
-In one study "4 patients who developed increased bone marrow reticulin on anagrelide showed regression of fibrosis when switched to hydroxyurea."
-"very little information exists regarding hydroxyurea’s effect on BMF"
The results of this study:
-"Despite the absence of JAK2 V617F mutation, our patient had a dramatic response to hydroxyurea as we have described"
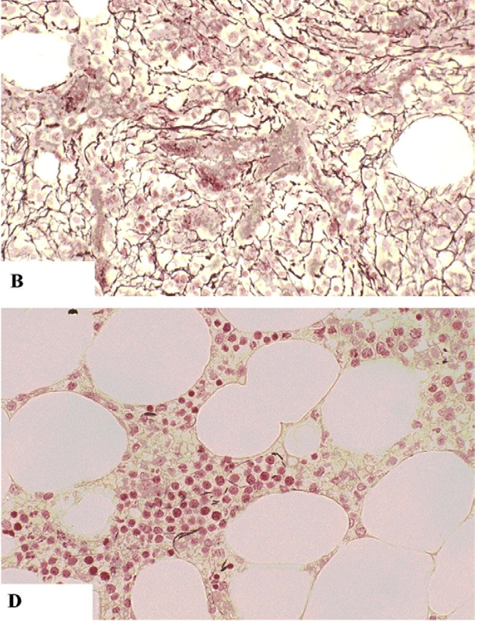
This BMB image in there shows obvious improvement to fibrosis. "B" has the dark stringy things (the fibers of high fibrosis grade), In "D" the strings are all gone (fibrosis of 0) after HU therapy. Cellularity also resolved (Figs A and C) but those images are harder to figure for us non-experts.