High/low JAK2 and Risk of MF progression - MPN Voice
High/low JAK2 and Risk of MF progression
Hi Manouche, as I am unfamiliar with graphs and the terms used on this one, could you explain the meaning/ results that are illustrated here? Many thanks!
This report is packed with info. I think it's from 2016.
Summary of interest:
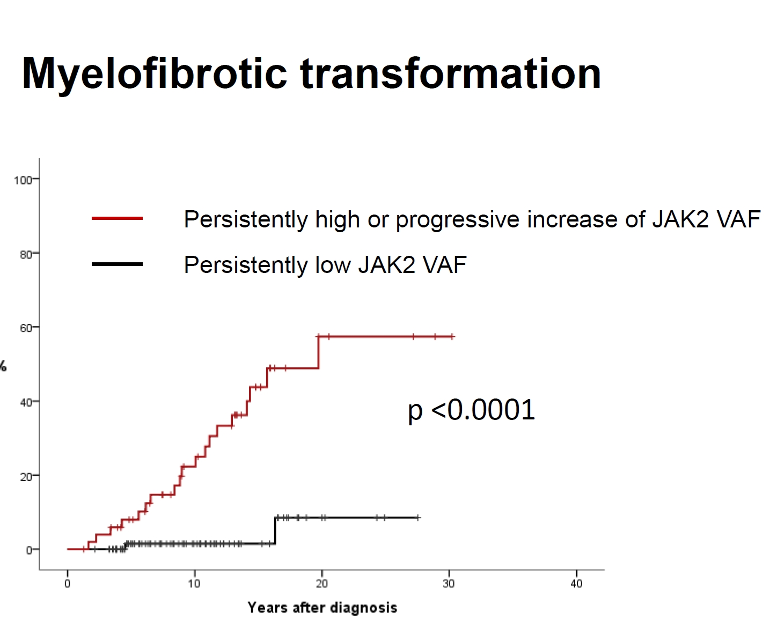
-Allele % (VAF) really matters for MF transformation (this is the plot Manouche posted)
-Any non-driver mutations are bad for AML at long periods (10-30 years), strongly so at 30 years.
-HU provide significant marrow improvements in some patients.
If you're at 2% VAF Jak2 on IFN, odds are good you can hold CHR off of IFN. But start IFN asap.
--
-For MF vs VAF I can't find a definition of low or high Jak2. Maybe cut off is 50%, maybe 20%? Clearly VAF really matters here with a hazard ratio of ~14 ie 14 times more likely to progress to MF with high VAF. But without a cut-off it's hard to make much of it.
--
-This part is clear, except the Jak2 cutoff is still missing:
NGS ET/PV conclusions:
• JAK2 VAF which increases or is persistently high correlates with risk of MF
• Mutations in other genes are involved with progression to AML but not to MF
• Non-driver mutations are found more frequently on patients with high or persistently high JAK2 VAF.
--
-So any non-driver at Dx has a quite negative AML prognosis at the very long time lines (20-30 years) By any they don't distinguish, but it appears that TET2 is not called out in the specific list. Non-drivers are much more important than Leukemogenic agents (assume to mean various chemos)
--
"Complete Histopathologic Bone Marrow Response at 12 months"
They list surprisingly good marrow improvements after a year on HU, example, half of ET patients had a complete response. In another study, IFN needs about 4 years to see marrow responses. Might it be good to combine them? This is not addressed. Maybe it's good to start on HU, as many of us did?
--
IFN discontinuation and keeping CHR, see plot:
Holding CHR off IFN without cytoreduction relates to: "........time between diagnosis and IFN start and mutant allele burden at IFN discontinuation remained jointly associated with the outcome."
Starting IFN ASAP after Dx helps. Stopping because of toxicity is a negative. Stopping with a VAF of not over ~2% is best. This is the left most line in the plot here. VAF of 40% at stop is worst.
--
Rux for MF:
Survival was 5.3 vs 3.8 years for no Rux. Benefit narrowed at 5 years.
--
AML transformed from MPN:
-No improvements in survival from 1989 to 2016, meaning treatments have not improved.
-
I’m sure there was a study posted here recently stating that >35% VAF for ET and >75% for PV were risk factors for progression.
Those would be high cut offs. I've also seen 50% being signif for PV. I tried to find the report this data came from but the PPT slides on this section have no ID info to search with.
I was wrong - apologies. 75% cut-off was the higher risk for thrombosis in PV. 50% implies homozygosity, so yes, a higher risk for progression.
This study covered both ET and PV. So that confuses the cut off even more. ET over 50% would be only a small portion. But the option of "increase" rather than "high" is easier to figure for either MPN since no cut-off level is required.
If there were a way to find this actual study likely we could figure it out better.
One of the biggest news in this report is the high rate for reversion of marrow in ET via HU. Strange this is not discussed more.
Thank you for taking the time to filter out this information from the 90 pages in this article. We all appreciate your efforts. Excellent work, thanks again from us all.