In this thread I made summaries of some of the videos that Hunter kindly provided.
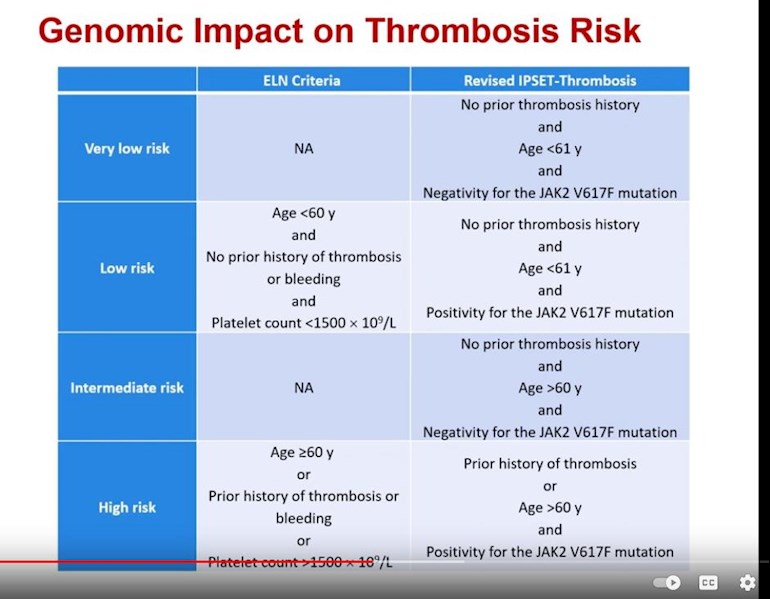
A top stand out item seems worth its own discussion. Raajit Rampal showed prior and current ET risk rating factors, see image. Here is my note:
"New ET thrombosis risk ratings: PLT counts are no longer in there. Used to be >150000, now not even listed. Jak2 status is now important."
The general idea is more focus on genetics.
There are very many posts on the Voice with concerns about PLT, does this mean we don't need to worry about it? (at least for ET)
Hunter added more context that was not in the posted videos, see here:
"As I recall Dr. Mesa also addressed this during the Q&A session. There is thinking that the value in cytoreduction for thrombocytosis is not in the absolute number, but in the delta (overall change in value). One of the docs also noted that the cytoreduction platelet target may need to be different for different patients. Some need a lower level than others based on actual symptoms that occur. "