It's confusing getting half a diagnosis.what does Ro-ve mean?
Results : It's confusing getting half a diagnosis... - LUPUS UK
Results
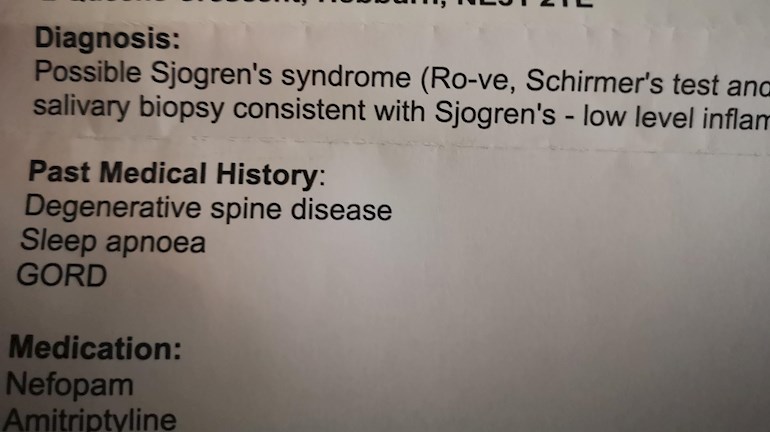
Hi Kels 🤗To me it says that you've been tested for sjogrens n that indications r that u have it..but you're Ro negative.
As I understand it a Ro+ is an indicator of SS. I'm ro+ n have just had the Schirmers test..I dont even know how to spell these things.. sorry!! 🙆
I've been told that I have some dryness..n been prescribed eye drops.
These things don't always show up in blood tests. There r many on here who r seronegative in blood terms but showing all symptoms of certain conditions. 🌈😽😽Xx
Hi Sue Petal
I have Ro 52 Antibody , yet my diagnosis is Sjowgrens over lap SLE .
My main consultants Speciality is Sjowgrens and he is a newly qualified consultant . I meet at of the criteria SLE .
Sometimes I think if you saw 6 different consultants with no idea about what the other had said . They may well come up with all kinds of overlaps , to include SLE an RA .
Myself , my joints are so bad and erosion seen on scans , yet no mention of RA .
I feel like I’m getting up from a car crash every morning . I’m so down with it all .
🦋❤️
If your lip biopsy was positive then that is enough to diagnose sjogrens without the bloodwork. It’s just called Seronegative and often affects people differently to seropositive. You shouldn’t be half diagnosed if your lip biopsy was positive as that’s the definitive test. Just wait and see what they say to you but with symptoms and lip biopsy these meet diagnostic criteria for SS.
Unfortunately not they said because all my other tests were negative, I don't fit all the criteria 😒
I think you need to find a decent rheumatologist who knows about sjogrens then. About 30% of people with sjogrens and rheumatoid arthritis are negative in blood. The positive lip biopsy and symptoms is what the rheumatolgist should go by - not just blood. Depending on whereabouts you live there are a couple of centres and specialists in the UK who have expertise in Sjogrens. I mean what’s the point of going to the trouble of having a lip biopsy if they are going to ignore the results? I feel most indignant for you!
Thankyou my schirmers test, ultrasound, saliva test and bloods were fine.They said I need at least 4/6 of results to be positive.My mouth, eyes and nose are all dry and I'm prescribed medication for that.
All those tests were normal for me too apart from that I had positive ANA. I still feel lip biopsy is the one they should go by as seropositve shows more in larger glands and seronegative often shows up differently.
Schirmers is a useless and unnecessary test my ophthalmologist says. The test they need to go by is the slit test where they use dye and measure the length between blinks or something. No optician or ophthalmologist would use a Schirmers to diagnose dry eyes.
Mouth - mine feels dry as a bone but isn’t, ultrasound was normal too. I’m still diagnosed with SS and it’s progressed to include another which shows in my bloodwork now too.
Sjogrens is a systemic disease like lupus and doesn’t always show classically as most general Rheumatologists seem to think. Can you get a second opinion from a sjogrens specialist I wonder?
I am already under a rheumatologist who specialises in sjogren's
Well in that case I guess they know what they should know what they are talking about🤷🏼♀️ Personally I’ve only come across one in the UK I trust on Sjögren’s and I occasionally see or speak to her privately.
hopkinssjogrens.org/disease...
From what I understand I agree with 282523 x
Thanks for this link dated 2021. I think the John Hopkins is probably the world centre for Sjogrens so I’d trust this page more than any others for the latest thinking. Very helpful to me as I have blood in my urine and no one knows why but it speaks about it here - first time I’ve ever read this. 😊
This might help the OP, Kells1974, take up the matter of positive lip biopsy as diagnostic of SS.
No mention of primary v secondary here either.
“Over the past 45 years, there has been an evolution in the definition of the symptoms and signs that, in aggregate, represent the disease process we call “Sjögren’s syndrome.” There is no single test that establishes the presence of this disease. Currently, the diagnosis requires either the presence of anti-SSA (Ro) antibodies or a biopsy of salivary glands from the lip showing a characteristic pattern of inflammation.”
Is the blood in urine caused by SS? What can they do about it x
I have written my Profile if you want to take a look - a few similarities x
The link you posted seemed to open on the blood and urine analysis part about SS I think? It was interesting to me because I’ve got renal ultrasound coming for permanent blood in pee. I’m sure, from reading this, that it’s not my kidneys themselves but the vessels/tubules that come off them. This seems to be a feature occurring in SS from this link?
I read your profile and yes some similarities I see.
But apart from hypothyroid and sjogrens my history is different as I have scleroderma in my blood and mine is mainly nervous system and vascular disease. I haven’t had the issues with being taken seriously that you seem to have had.
Sorry you’ve had it so hard getting correctly diagnosed😊x
Ah yes, that was meant to be that you got that link then! 😄 I sent it because it talks about the high pecentage of people with negative antibodies but have SS all the same x
Yes definitely meant to be! I then clicked on diagnosis on your link and it clearly states the only way of formally diagnosing SS is antibody bloods or lip biopsy. So still very confused on behalf of the poster here on why their so-called sjogrens expert Rheumatologist is doubting their diagnosis- when this result is positive for SS according to the 2021 diagnostic criteria set out by the leading SS centre in the world - at John Hopkins? x
Yes exactly x
Just to let you know that my saliva and ultrasound were both negative but schirmers test produced different results on two seperate occasions. Nevertheless, they still proceeded with a lip biopsy that came back positive for secondary Sjogren's.
I would definitely try and get a second opinion.
Good luck!
Exactly the same happened with me. However I had a BSR email notification today confirming we have Sjögren’s - the primary and secondary classifications no longer apply now I’m glad to say😊
“The new ACR/EULAR criteria no longer distinguish between primary and secondary SS and we will thus address the management of SS as a single entity but comment on management of overlaps where appropriate”
academic.oup.com/rheumatolo...
The management of Sjögren’s syndrome: British Society for Rheumatology guideline scope
Elizabeth Price, Alexander Allen, Saaeha Rauz, Anwar Tappuni, Nurhan Sutcliffe, Michele Bombardieri, Sara Carty, Coziana Ciurtin, Bridget Crampton, Lisa Duncalfe ... Show more
Rheumatology, keaa870, doi.org/10.1093/rheumatolog...
Published: 02 February 2021
I had been tested via ANA since my twenties for typical Lupus symptoms, hair loss, Raynauds, repeated sinus infection as well ear infection (like the little kids get!). I developed autoimmune thyroiditus. They discovered anticardiolipins when tested again for Lupus still ANA negative in my fourth pregnancy and I took aspirin for the remainder and developed pre-eclampsia and was induced at 36 weeks. Several years with joint pain and I just thought this is what it feels like to be in your forties with you g children LOL. Several years after having my last child I developed a very dry mouth & was still dealing with Raynauds & was having a lot of eye pain and significant blurring. My eye doctor wrote an order to my primary care to test ANA (still negative) plus SSA-Ro (high positive) and then I was referred to a Rheumatologist.
I was diagnosed with Lupus with Secondary Sjogrens despite being ANA negative (apparently less than 3% have a negative ANA but they typically are positive for the SSA-RO autoantibody). I was put on 400 plaquenil & have been followed 4 times a year by a rheumatologist for blood/urine tests. Within 3 years of diagnosis I became ANA positive with a number of other autoantibodies showing up & going down. fFive years later plaquenil reduced to 350 mg under new Opthamology guidelines in order to prevent tocular toxicity.
In the last few years I finally developed anti double stranded auto DNA and very high levels of certain anticardiolipins for which I again take an aspirin. In addition my Complement C3 dropped. I also have bone erosions which is not typical of Lupus and my rheumatologist suggests “rhupus”. I also have high neutrophils and low lymphocytes which are said to be typical of Lupus.
I believe that I had Lupus since my mid twenties when I had my first round of hair loss and severe migraines only relieved by prednisone but due to the negative ANA I did not get the diagnosis for another twenty years.
I currently take 350 mg plaquenil, 30 mg cymbalta (great for arthritic pain, enabled me to start exercising again, I could not tolerate any dose high than that but this dose works for me), 2 mg prednisone daily, 5 mg adderal for “lupus fog” & lupus fatigue (life-changing). I also take Advil for pain several times a week and I am currently trying a CBD gummy at night to see if it improves my sleep which can be interrupted due to aches and pains.
It has take me many years to find what works for me. I did try methotrexate with disastrous results (after second weekly injection lymph glands swelled in my neck cause a lot of pain. I also developed a strong metallic taste in my mouth which was totally offputting for eating and took a month to go away after stopping the injections. I lost 8 pounds during that month, brushing you teeth all the time made NO difference. Over the last three months I have been considering trying Benlysta (doctor already approved) but I have decided to hold off due to Covid.
You bet! Back when Inwasnin my twenties I didn’t even know what Lupus was and after the hair loss when the doctor said you don’t have LuousnInwas always surprised, hey what is Lupus but you know I never asked!
I believe this information you have been given is now considered out of date.
EG I have systemic scleroderma in my blood and sjogrens diagnosed by lip biopsy before the scleroderma arrived. No rheumatologist is calling mine primary or secondary anymore - they just say I have both.
Why should Sjogrens be primary or secondary anymore than lupus, RA or scleroderma are??
Information given out online needs to be updated. The overall impact of dryness is often multisystemic. For some the dryness isn’t even felt much and sjogrens can often be mistaken for MS or RA or Lupus because this is how it initially presents. This doctor explains:
“Not secondary- words matter.
Sjogren’s does not get the attention that it deserves. Words that are used to describe Sjogren’s contribute to the neglect of this common and serious disease. Patients with so-called "secondary Sjogren's" are even more likely to have their disease downplayed or dismissed.
This blog post explains how the term "secondary" feeds into the misperception that Sjogren's is not as important as other major rheumatologic diseases.
Tips for talking with rheumatologists: You will find a few ideas in the blog post about how to talk to your doctors about their view of Sjogren’s. This is an important first step for discussing your Sjogren’s care.
Sarah Schafer, MD and Sjogren's patient”
And top of a quick google search
Sjögren's Foundation
Sjögren's is a systemic autoimmune disease that affects the entire body. Along with symptoms of extensive dryness, ...”
It does look like experts in these diseases are advocating for clearer diagnostic categories. What I read is proposed SS or SS associated with another autoimmune disease.
Primary or secondary does seem like a problematic way to categorize.
Thanks for drawing our attention to this. Times have really changed. I diagnosed my own Sjogren’s. 😅. Then my anti LA antibodies became positive during regular rheumatology follow up.
Keep us posted!
Xk
Thanks KayHimm. I’m struggling with secondary depression and secondary oral thrush that is ongoing and seems to have infected my entire body system now all due to Sjogrens disease so I’m not in the mood for anyone who thinks that Sjogrens begins and ends with dry eye, mouth and vagina. Bodies aren’t made to have secretory glands attacked. I read such suffering and so many affected by misinformation about sjogrens online. It really hurts. Thanks for your open mindedness. I self diagnosed scleroderma and lupus years ago and scleroderma is now official!
When my rheumatologist returns after being redeployed for Covid - I’ll show her photos of my new butterfly rashes. But diagnosed or not with lupus it won’t make much difference as both sjogrens and scleroderma can and do harm the internal organs too. My treatments wouldn’t change either. X
Oh, yes, both can be devastating. They are among the rarer autoimmune diseases. I know of a woman with Sjogren’s (friend of a friend) who moved her family to Baltimore from Canada to get care at John’s Hopkins. She has two children and struggling with severe neuropathy. IVIG is partially helping. There is no question these are life-changing illnesses.
There was an article in the NYTIMES about the under-appreciated and under-diagnosed aspects of Sjogren’s.
All of these diseases can do damage. No debate about that.
I always wonder how a person couldn’t be depressed with what we go through with diagnosis that can take a quarter of a person’s life and facing a future that will never be like the past.
Do hope you have a good appointment with your consultant.
Xk
No idea. I don’t use this HU very much. Is this person up to date? I have Overlap Syndrome - may or may not include Lupus. I only know about Sjogrens because it’s the one that affects me most at the moment so I read a lot about it.
My understanding is the reason they have differentiated between primary and secondary Sjogren’s was for research purposes. I don’t know where it stands now but primary Sjogren’s was thought to be more severe.
These classifications change as more research is done and better diagnostics tools are developed.
Hot off the press today! 😊academic.oup.com/rheumatolo...
That’s a shame I wonder why it isn’t opening for you? I’ll see if I can copy and paste some relevant extracts.
“The management of Sjögren’s syndrome: British Society for Rheumatology guideline scope
Elizabeth Price, Alexander Allen, Saaeha Rauz, Anwar Tappuni, Nurhan Sutcliffe, Michele Bombardieri, Sara Carty, Coziana Ciurtin, Bridget Crampton, Lisa Duncalfe ... Show more
Rheumatology, keaa870, doi.org/10.1093/rheumatolog...
Published: 02 February 2021 Article history”
“introduction
Why the guideline is needed
Healthcare workers often underestimate the burden of Sjögren’s syndrome (SS) and people with SS struggle with the chronicity of the condition and are frustrated by the paucity of treatment and lack of knowledge in the medical world. This will build on previous guidelines and continue to address these issues.
The most recent British Society for Rheumatology (BSR) guidelines on SS were published in 2017 [2]. Since then, the monitoring guidelines on hydroxychloroquine have changed, new eye drops have come to the market and research into the underlying mechanisms of disease has progressed, with new treatments being trialed.
There are existing international treatment recommendations that may be applicable in the UK including those published by the EULAR in 2020 [3] and the North American guidelines published in 2016 [4]. However, these are generic to many international health settings and do not provide specific guidance for the UK, nor do they include the management of children. This guideline will aim to address management in both adults and children and will focus specifically on the healthcare setting in the UK. In doing so it will take into account issues specific to the UK-based population, the majority of whom will access healthcare through the National Health Service (NHS). It will advise on best practice standard of care within the UK and cover the patient journey from initial presentation to diagnosis and long-term management, taking into account specifics such as UK access to drugs.”
“More severe clinical course and higher risk of lymphoma development [7, 8].The physician should aim to empower the individual to manage their condition; conserving replacing and stimulating secretions; preventing damage and suppressing underlying systemic disease activity.
SS has a significant impact on the quality of life (QoL) of affected patients. A recent literature review found that health-related (HR) QoL was markedly reduced in SS in multiple studies across many countries when compared with healthy controls [9]. The reduction in HRQoL was similar to that observed in other chronic diseases such as rheumatoid arthritis and lupus, suggesting that it is not a ‘benign’ disease. This reduction in QoL has been noted in multiple domains and across all populations studied worldwide. Anxiety, depression, pain and fatigue are all increased in SS compared with healthy controls and significantly impact on the QoL [10]. The loss of taste and smell that accompanies SS has a negative effect on the QoL [11] as does the ocular dryness [12, 13]. There is a significant reduction in sexual QoL [14] due to the combined effects of vaginal dryness [15] and atrophy [16]. Systemic involvement, including nervous system disease such as peripheral neuropathy [17] and respiratory system involvement [18] also have a negative impact on QoL”
“ The new ACR/EULAR criteria no longer distinguish between primary and secondary SS and we will thus address the management of SS as a single entity but comment on management of overlaps where appropriate.”
Thanks! Yes, the experts certainly have set out to change the understanding and treatment of the disease. I noticed there is a rheumatologist at the hospital where my doctors are affiliated who treats only Sjogren’s patients. That sort of marks a change, right?
The largest hospitals in New York seem to have Sjogren’s clinics. I don’t know if that is new or not.
Looks like there is a move forward.
Karen
Yes it’s all very promising I agree Karen 😊
“The new ACR/EULAR criteria no longer distinguish between primary and secondary SS and we will thus address the management of SS as a single entity but comment on management of overlaps where appropriate”
academic.oup.com/rheumatolo...
The management of Sjögren’s syndrome: British Society for Rheumatology guideline scope
Elizabeth Price, Alexander Allen, Saaeha Rauz, Anwar Tappuni, Nurhan Sutcliffe, Michele Bombardieri, Sara Carty, Coziana Ciurtin, Bridget Crampton, Lisa Duncalfe ... Show more
Rheumatology, keaa870, doi.org/10.1093/rheumatolog...
Published: 02 February 2021
So does this mean,I should get a diagnosis on the results of my positive lip biopsy alone?
Yes it does if you have symptoms too ie joint pain, dryness of eyes and mouth (see optician not rheumatologist) or neuropathy or GI issues. You also have raised inflammation I think so I just can’t understand why you haven’t been diagnosed? If not antibody positive then lip biopsy is the most definitive test and is used to diagnose Sjögren’s. I’ve been baffled by this ever since reading your post!
Thanks yes, I get eye drops and saliva spray on prescription.I have dry nasal passages,mouth ulcers gerd and joint pain.
Then I think you’ll have to send the EULAR diagnostic criteria or this newly published BSR paper to your rheumatologist and ask why they aren’t diagnosing and treating you now in keeping with the critera and newly published BSR guidelines on SS.
I had normal ultrasound and schirmers and spit test 6 years ago but my lip biopsy was fully positive so I was diagnosed. Seronegative often presents differently. But the other tests done by rheumatology aren’t definitive because they are too basic. Only optometrists and dentists can diagnose dry eyes and mouth, not rheumatolgists - they don’t have the equipment. You could go back to your optician and ask for a dry eye slit test. If this shows dry eyes then ask them for a letter confirming this to show your rheumatologist. SS doesn’t always start in eyes and mouth.
Ps I’m in similar situation with systemic sclerosis - only opposite to you in that my specific antibodies are very positive but my nailfold capillaries are normal so the scleroderma rheumatologist says I don’t fit the criteria yet. So I understand your frustration. But if you read diagnostic criteria then you have SS and I have systemic sclerosis overlapping my SS. Mine is called Overlap CTD.
I hope you fit the criteria soon.
Thanks. I do actually already fit it according to my new consultant, my dermatologist and the sjogrens expert I saw privately. But the latter described it as a “heart-sink” diagnosis as there’s no real modifying treatment and it’s the most potentially life threatening serious rheumatic disease so I’m relieved if I don’t have it yet! SS and Lupus are a far better diagnosis’s she said.
But like your rheumy, the scleroderma rheumatologist is being a bit rigid and wanting me to fit into a box I probably never will fit.
I’m the only one one in my area, with this scleroderma antibody so she wants me back. From my perspective she doesn’t know enough about Sjogrens and how my overlap works - maybe because it’s all so rare she’s never seen it before. I’m on the right treatments already.
In my opinion what matters is to find better rheumatologists who can think outside the box. For example I’ve found someone in Wales who carries the same very rare antibody as me and her rheumatologist (her third) has diagnosed her with Scleroderma on the strength of symptoms and this antibody. Like me she had no nailfold capillaries changes.
If we have overlaps of early stages of one of these autoimmune diseases we may not show classically. So I’m going to have to go back to the scleroderma rheumatologist now because my Lupus rheumi has to defer to her colleague on Scleroderma. I hope I don’t have it yet but increasingly I have symptoms and signs.
If your rheumi won’t diagnose you despite you meeting the criteria (which I believe you do) then my advice would be, politely move on because they clearly are too rigid a thinker. X