An interesting review focused on IgG that is clear, concise and simple.
Click on the link -
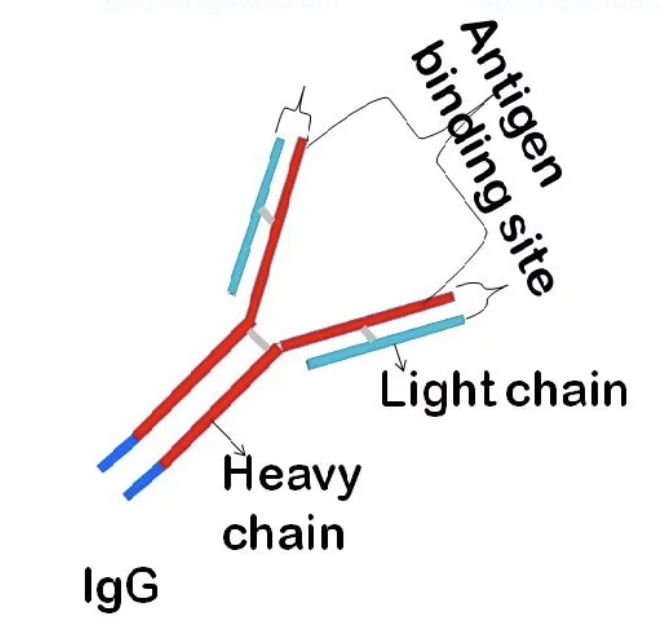
An interesting review focused on IgG that is clear, concise and simple.
Click on the link -
Yes it’s very illustrative. I’d just bookmarked it earlier 😉
Having hypogammaglobulinaemia, it’s a subject of great interest to me. I was surprised to read that low immunoglobulins can be responsible for persistent diahorrea. It’s something I intend to discuss with my specialist.
Newdawn
It seems that many of us with cll and low Ig's experience G.I challenges.
Seemingly true but I’m not sure the link is always accepted Smakwater.
Newdawn
I'm wondering if the GI challenges are more related to low IgA than IgG, given secretory IgA's (sIgA) important role in protecting our mucous membranes. "sIgA is the main immunoglobulin found in mucous secretions, including tears, saliva, sweat, colostrum and secretions from the genitourinary tract, gastrointestinal tract, prostate and respiratory epithelium. It is also found in small amounts in blood. The secretory component of sIgA protects the immunoglobulin from being degraded by proteolytic enzymes; thus, sIgA can survive in the harsh gastrointestinal tract environment and provide protection against microbes that multiply in body secretions.[6]"
en.m.wikipedia.org/wiki/Imm...
Per When Therapeutic IgA Antibodies Might Come of Age
karger.com/pha/article-abst...
"Furthermore, secretory IgA is emerging as a major regulator of gut microbiota, which impacts intestinal homeostasis and global health as well. As such, IgA could be used to promote a healthy microbiota in a therapeutic setting."
The company producing Hizentra were investigating producing an IgA infusion product, but I don't know what's become of that initiative. Also IgG can substitute somewhat for IgA and has a longer half life of around 3 weeks, compared to the 4 to 7 days for IgA.
Interestingly, the amount of IgA in IgG infusion products is carefully controlled. It's actually filtered out, because some patients (though not those with CLL that I know of), are more likely to have severe infusion reactions (anaphylactic shock) from the IgA. Again per the earlier Wikipedia reference, "Anti-IgA antibodies, sometimes present in individuals with low or absent IgA, can result in serious anaphylactic reactions when transfused with blood products that incidentally contain IgA. However, most persons with suspected IgA anaphylactic reactions had experienced acute generalized reactions that were from causes other than anti-IgA transfusion. "
Thanks for the post, Smakwater. The Patient Power article does indeed provide a clear explanation.
With respect to the final sentence of the article" Subcutaneous (injected under the skin) immune globulin is also offered, works similarly to IVIG, and may be less costly." It should be less costly, given it is self administered, but in the USA that very much depends on your health insurance provider. Subcutaneous IgG provides more even protection over time, as you typically infuse it weekly into a pocket under your abdominal skin, from which it gradually infuses into your blood. So you don't get the big spike into your veins you get with IVIG. Subcutaneous IgG also saves your veins. 
Neil
Yes I think you’re definitely onto something there Neil in relation to the role of the IgA. The paragraph header gave the impression they were connecting the GI issues to depleted IgG but then widens it to include the impact of low immunoglobulins across the board;
Will I Have Symptoms if My IgG levels Are Abnormal?
‘When people have low immunoglobulin levels, the first indication may be repeat infections, such as throat, sinus, ear, or respiratory viral infections. People may also have chronic diarrhea.’
My IgA and IgM are severely depleted.
Newdawn
I have hypo-gg too, since finishing FCR treatment 3.7 years ago, and with globulin levels static over that time I guess it's chronic. Or is it? End of my treatment coincided with the arrival of Covid, and new era of isloating, masking and handwashing, i.e. avoiding exposure to pathogens. No exposure => no new Igs, right?
Remember that you are constantly exposed to new pathogens in the air you breathe, as well as what you drink and eat. You don't live in a sterile environment.
Neil
I, like Neil am not convinced the isolating phenomenon has significant impact on levels but it’s an interesting hypothesis. (I shielded religiously for a long time and caught Covid at home after a fleeting visit from someone in full protective gear!)
My IgG’s ‘recovered’ marginally following the end of treatment in ‘21 but are on the decline again now. It’s only recently that I’m beginning to wonder if this chronic and long standing immunoglobulin deficiency (across the board) is impacting my health generally. It feels like my body is on constant ‘high alert’ without the buffer that IVIG offered. However, the criteria for receiving infusions is very much confined to CLL type issues on the NHS and not holistic health deficiency.
Newdawn
Thanks Newdawn.
Did you have your IGs tested before treatment or like me only during and after? I've always assumed that the hypo-gg was treatment-induced, but studies have found it abounds in newly diagnosed CLL patients (mostly at a more advanced stage of disease) e.g. ncbi.nlm.nih.gov/pmc/articl... and onlinelibrary.wiley.com/doi...
I would like to think that the health service is doing its best for you, though I realise that long term IVIG is too much to expect by way of symptom management. There may be a link with Ig deficiency, which has been demonstrated when it comes to PID. For myself, although my IgG and A were well below reference at the last count, the only consequence seems to have been that when I caught a RSV or a severe cold it took 3 or 4 times longer than "normal" to get rid of the symptoms, though from the latter developed a chest infection requiring 2 sets of ABs to clear.
Testing immunoglobulins is of course pretty unheard of as a standard test in the NHS unless some serious primary deficiency is suspected and that tends to develop at an earlier age. However, I recall the haematologist I ‘sacked’ looking concerned about mine about a year into W&W. Incidentally I’d had to insist he checked them. He then exclaimed that I’d need an urgent BMB and when I asked him the rationale behind that he couldn’t explain. I insisted on changing to another haematologist that day.
I suspect they’d started depleting slightly prior to dx…the chicken and egg situation. They continued to drop throughout my 7 yrs of W&W and by treatment I needed IVIG pretty urgently. I had repeated and severe respiratory infections. I was hospitalised with pneumonia and sepsis.
The IVIG was given monthly for a year until Covid time and with an IgG of 4.4, I no longer qualified 🙄 Plus I was then on prophylactic antibiotics as part of the trial.
Interestingly, no matter how good my other labs look, my immunoglobulins still do their own thing. However, I can only imagine I have robust T cells because I’ve faired quite well generally in terms of dangerous infections including Covid (touching wood quickly) 😉
Newdawn
Great explanation. Thanks for sharing!
Hi Smakwater, Once again this is a topic right at the top of my concerns. Like Newdawn, I too have a diagnosis of hypogammaglobulinaemia and am now in my 11th year of 3 weekly IVIG infusions and although my IgG is generally in range my IgA and IgM hardly register.
I should add that during the Covid pandemic and lockdown I did miss two infusions which led to my IgG falling below the then UK threshold.
I do also suffer from repeated sinus and ear infections and have just finished a course of antibiotics for an infection in my big toe.
Also of interest is the suggestion that low immunoglobulin’s might be responsible for my chronic ongoing issues with diarrhoea. This problem was always blamed on my Behcets Syndrome, (Behcets now regarded as a disease) as are my ongoing gastric issues.
All in all a very interesting article.
My regards
Aerobobcat