Yesterday arrived a letter from my local NHS Hospital Trust. I get them quite often, and as it happens I was anticipating an appointment with a physio about now.
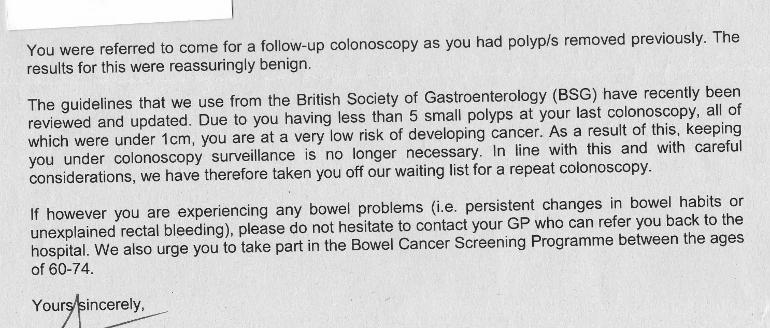
But no, this one was more of a "dis-appointment". A letter from the Department of Colorectal Surgery was overdue, I thought, but as you can see from the above, that appointment is no longer necessary - now or ever - as I am no longer considered at unusual risk of developing colon cancer. Furthermore, I'm even considered "at very low risk" of developing colon cancer. Nice to know!
Now, we can debate the secondary cancer risk level of a CLL patient with a family history of colorectal cancer, and with sessile polyps found at each of the last two colonoscopies. What is beyond debate is that "the polyps at your last colonoscopy" were not "under 1 cm" (as the colonoscopy report confirms, and the report from 5 years previously adds emphasis). One therefore marvels at the temerity of the concluding sentence: "In line with this and with careful considerations, we have therefore taken you off our waiting list for a repeat colonoscopy".
Having lost one sister and one dear friend to bowel cancer diagnosed at an advanced stage, this is a bit of a hobby horse for me.
The UK's dismal record of cancer mortality due to late diagnosis was highlighted on BBC Radio 4 this morning in an interview with Shadow Health Secretary, Wes Streeting. Bowel cancer - in 2017 the second most numerous killer of all the cancers in the UK - contributes greatly to this unhappy state of affairs, despite the widely canvassed Bowel Screening Programme for the "at-risk" 60-74 age group.
This national programme is based on faecal immunochemical testing, which screens for concentration of faecal haemoglobin (f-Hb). Research in 2020 called out the current screening programme, in that the f-Hb threshold used in England was estimated to identify only 47.8% of bowel cancers (CRC) and 25.0% of high risk polyps (HRA) journals.sagepub.com/doi/10... and evidence.nihr.ac.uk/alert/n...
The recommendations of this study are not as straightforward as lowering the f-Hb threshold to a level that would identify many more cancers and potential cancers, say 82.2% of CRC and 64.0% of HRA, because that would imply offering 7.8 % of all participants screened further investigation by sigmoidoscopy and/ or colonoscopy. Instead the researchers recommend multi-level f-Hb thresholds leading to different screening pathways mostly involving delayed screening or surveillance; only in the event of "high blood concentration" would a standard colonoscopy be offered. The proposed system takes no account of pre-existing polyps, familial history of CRC, or statistical likelihood of developing a secondary cancer because of immunosuppression.
It seems to me that the above proposals are an as-yet untested refinement of the current f-Hb based screening programme, which might or might not pay dividends. We shall see, but one suspects that the NHS budget will be the principal benefactor.
Meanwhile, I'll be composing my response to the offending letter.