1. The risk of developing a Secondary Primary Malignancy
"The higher risk of SPM associated with CLL has been recognized for many years, well prior to the modern therapy era. Manosow and Weinerman in 1975 demonstrated a three-fold increase of SPM and an eight-fold increase of SC in CLL"
Thus reads part of the introduction to a 2021 study of SPMs (secondary primary malignancies, i.e. secondary cancers, whether solid tumours or blood cancers) including SC (skin cancers) in a cohort of 517 CLL patients onlinelibrary.wiley.com/doi...
Since 1975, many studies have shown Manosow and Weinerman's estimates to be exaggerated, or one could say "no longer applicable". For Part 1 of this post I've chosen a fairly recent, large-scale study from the Netherlands to explore how the risk of developing another cancer is affected by a CLL diagnosis. The study nature.com/articles/s41408-... compares the incidence of second primary malignancies (SPMs) among 24,815 CLL patients diagnosed during 1989-2019 in the Netherlands with the expected number of malignancies in the age-, sex-, and period-matched population. The relative risk, as expressed by the standard incidence ratio (SIR) observed, was 1.67 in solid cancers (95% CI, 1.65–1.75) and 1.42 (95% CI, 1.24–1.62) in blood cancers. That means, across all solid tumours, a CLL patient has on average a 67 % higher chance of developing a (second) primary cancer than their counterpart in the general population, and a 42 % higher chance of developing another type of blood cancer. So, nowhere near the threefold risk proposed in 1975.
Although this finding is in line with earlier large scale studies in the USA, Denmark and Australia, the overall relative risk of getting cancer is not an especially useful number to know. We need to understand our absolute risk levels too, and for different types of second cancer, especially the ones that tend to afflict our gender and age group and are life-threatening.
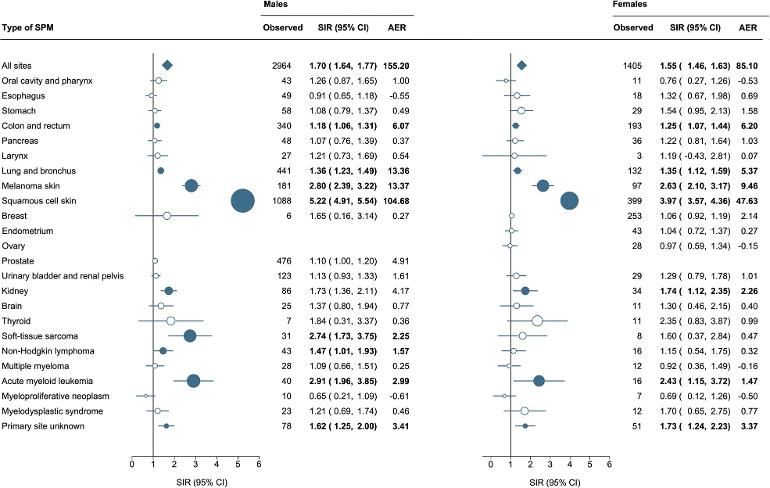
This recent study presents its findings in the form of "forest plots" with data rows alongside, giving the reader an instant visual impression, plus statistical measures of the relative risk (SIR) and the increase in absolute risk (AER) for each type of cancer. Reading these plots is easier than it sounds! Browse the Figures in the article, showing forest plots of different SPMs for CLL patients in the study, according to sex (Fig 1), age (Fig 2), latency time i.e. between diagnoses of CLL and SPM (Fig3), and receipt of antineoplastic therapy i.e. chemotherapy (Fig 4). Also, read the commentary above each Figure.
A number of interesting conclusions emerge:
• Overall, CLL males have a higher relative risk than CLL females of a SPM: SIR 1.70 v 1.55, but because they are more prone to cancer in the general population, CLL males have almost twice the absolute excess risk of a SPM compared with CLL females.
• The absolute risk of a SPM tends to increase with age, while the relative risk of a SPM tends to level off after the age of 60.
• Numerically, by far the most significant SPMs are skin cancers, particularly non melanoma types; the SIR for all skin cancers would exceed 3 (Fig 4).
• Other SPM risks of note are colon, lung and kidney cancer, and soft tissue carcinoma, all with SIRs in the range 1 to 3.
• For several of the SPMs listed the absolute excess risk (AER) is modest to negligible, e.g. myeloid blood cancer, breast, ovarian and endometrial cancers.
• Excess cases of acute myeloid leukemia (AML) seem to be wholly driven by myelodysplasia (MDS) following chemotherapy (Fig 4), although before 2003 and in patients over the age of 70 this chain of events is absent (Fig 2).
• Chemotherapy also increases the risk of skin cancers (Fig 4).
So I'm at risk - what can I do about it except worry?
CLL is an exception, but with other types of cancer the key to survival is early diagnosis. And you can still make choices that should lessen your risk of developing a particular type of SPM.
Skin cancers - the most significant class of SPM for CLLers - are very amenable to early diagnosis and treatment, malignant melanoma being the most feared. Frequent self examination, preferably with the help of a partner to scrutinise your back, in between regular dermatology consultations, is essential.
...and of course, you can reduce your chance of developing skin cancers by covering up while you are outdoors on a sunny day.
Colon cancers tend to be slow growing but symptoms can be vague. CRC screening programmes based on FIT cancerresearchuk.org/about-... are worth doing, though in some countries (UK) the haemoglobin cutoff level is so high that it means that half of carcinomas and three quarters of precancerous adenomas are missed. So it's a good idea to get yourself on a 4 or 5-year schedule of colonoscopies or, failing that, virtual colonoscopies (low dose CT scan), which even the NHS offers, sometimes.
...not forgetting that maintaining a healthy diet can reduce your risk of developing colon cancer.
Lung cancer - apart from smoking, which accounts for 80 % of lung cancer deaths, there may be other primary risk factors that you can change in your favour, see cancer.org/cancer/types/lun...
For other cancers there may be no excess risk of a SPM due to CLL, but don't neglect any community health screening progammes and regular health checks that are on offer.
If these things make you gulp just thinking about them, just remember this:
Fear is a vital emotion designed to spur us into action
Worry/ stress/ anxiety is a state brought on by inaction
Go well.
Edit
A couple of the replies to this post have prompted an addendum.
This post is concerned with the relative risk, or the absolute excess risk of getting a second cancer for those with CLL. It says nothing about your baseline risk, i.e. the absolute level of risk that exists for each type of cancer in the general population. Some of the SPMs mentioned in the study article, e.g. breast, lung and colorectal cancer, are much more prevalent generally than the likes of pancreatic and kidney cancer, see wcrf.org/cancer-trends/worl...
That said, your individual risk may be very different from the average in the population. Genetic risk factors like ethnicity and inherited predisposition are clearly beyond your control; while certain environmental and lifestyle factors may be things you can influence, to swing the odds in your favour.

 Just to clarify, my mother and I were tested, and neither of the BRCA genes were found, BUT the geneticist said that with the close cluster of cases in our family, there was likely to be something else genetic going on that hadn't yet been identified. Things may have progressed in the 20-ish years since, of course.
Just to clarify, my mother and I were tested, and neither of the BRCA genes were found, BUT the geneticist said that with the close cluster of cases in our family, there was likely to be something else genetic going on that hadn't yet been identified. Things may have progressed in the 20-ish years since, of course.