My Story: I have restarted ADT treatment, after a RP and after RT and without evidence of rising PSA (mine is undetectable). My current Urologist stressed that my cell type via the Decipher test shows a very aggressive cancer type and that my margins were 60% Gleason 4...further, that that I should not have been taken off ADT during and after RT...and that I should stay on ADT for 2 years after my RT...I had requested this from my Oncologist after the end of my RT not knowing why, but was rebuffed...although its not certain how long post RP - post RT ADT should be given (see attachments), its most certainly shown in this article that salvage ADT improves your chances of preventing BCR post RP - post RT...therefore, I have started on a 2 year treatment with Lupron...so far so good...article follows.
Background: Assessed the influence of androgen deprivation therapy (ADT) during and/or after post-prostatectomy radiotherapy (RT) on biochemical recurrence (BCR) and radiographic progression in patients with prostate cancer.
Methods: Patients with prostate cancer who underwent post-prostatectomy RP, radiation treatment RT were analyzed. BCR bio-chemincal recurrence and radiographic progression (rising PSA) after RT were compared according to the concurrent or salvage use ADT.
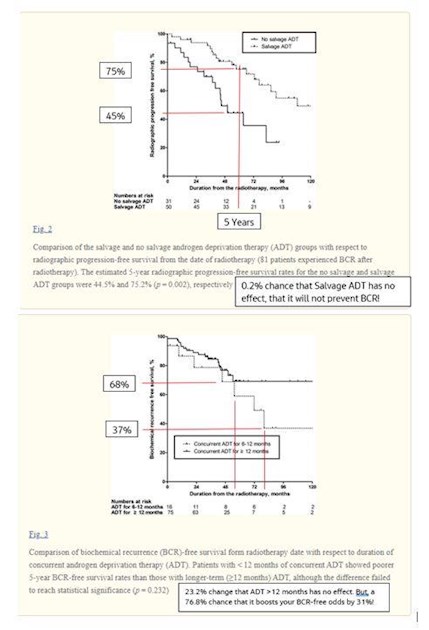
Results: Of the 227 patients who underwent post-prostatectomy RP, RT, 95 (41.9%) received concurrent ADT for a median of 17.0 months. Despite more aggressive disease characteristics in the concurrent ADT group than in the RT-only (no ADT) group, the former had a better 5-year BCR-free survival rate than the latter (66.1 vs. 53.9%; p = 0.016), whereas the radiographic progression (post RT PSA) rate was not significantly different between two groups. On the other hand, salvage ADT after post-RT BCR significantly delayed radiographic progression than the non salvage ADT group (5-year radiographic progression-free survival; 75.2 vs. 44.5%; p = 0.002).
Conclusions: Concurrent ADT improved BCR-free survival, and salvage ADT after post-RT BCR improved radiographic progression-free survival. To maximize the oncological benefit, ADT of sufficient duration should be implemented.
Definitions: terms used are defined.
a. Adjuvant RT was the administration of RT to RP patients who had adverse pathologic characteristics (pT2 with positive surgical margins, pT3, or pN1), prior to the PSA recurrence.
b. Salvage RT was the administration of RT to patients with PSA recurrences after surgery without evidence of systemic disease
c. Supplementary ADT was classified into concurrent and salvage ADT according to time of administration.
d. Concurrent ADT was defined as ADT administered before, concurrent with, or after RT.
e. Salvage ADT was defined as ADT administered after a post-RT BCR.
f. Radiographic Progression was defined as either Response Evaluation Criteria In Solid Tumors (RECIST) or bone scan progression defined as two or more new lesions at the initial after treatment assessment confirmed by additional lesions ≥6 weeks later, or two or more new lesions at any time beyond the initial post-treatment assessment, which accounts for the potential misclassification of bone progression due to osteoblastic healing. (Ref B)
Details: Despite the stage migration in prostate cancer noted in this prostate specific antigen (PSA) screening era, extra prostatic disease continues to occur in more than one-third of patients who undergo radical prostatectomy (RP)
a. Results from the RTOG 9601 showed that adding a 24 month anti-androgen (AA) treatment during salvage RT reduced mortality over a median follow-up of 12.6 years compared with salvage RT-only treatment (12-year overall survival [OS]: 76.3 vs. 71.3%
b. The GETUG-AFU 16 trial demonstrated that 6 months of luteinizing hormone releasing hormone (LHRH) agonist treatment during salvage RT significantly reduced clinical progression (5-year progression-free survival, 80.0 vs. 62.0%).
c. This study assessed the oncological benefit of supplementary ADT during or after post-prostatectomy RT.
d. With respect to ADT duration, we found that patients who underwent < 12 months of concurrent ADT showed poorer 5-year BCR-free survival than patients who underwent longer-term (≥12 months) ADT, although the difference failed to reach statistical significance (p = 0.232; Appendix). These findings concur with the results of a previous study [23]. These findings suggest that the concurrent ADT duration should be extended to 12 months or longer.
e. When post-RT BCR occurs, salvage ADT may be considered a viable treatment option in patients with hormone-naïve or hormone-sensitive prostate cancer.
f. The RTOG 9601 study protocol stated that salvage ADT should only be administered when there is radiographic or pathologic evidence of metastatic disease. The administration of salvage ADT was not restricted in this way in our study
LINKS: articles