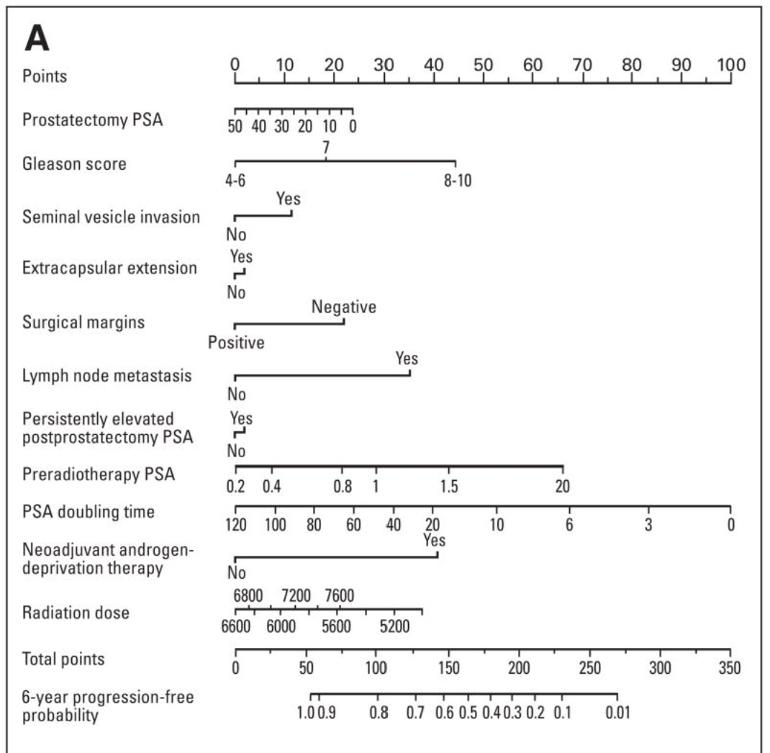
Summary: Patients in this audience have had both radical prostatectomies (RP) and salvage radiation treatment (sRT) and want to know their chances of having recurrent prostate cancer. This study developed a predictive model called a nomogram that predicts the 6-year progression-free probability (PFP) after SRT for men with PSA recurrence after RP. The model used to predict the probability of disease progression after SRT is taken from a multi-institutional cohort of 1,603 patients. The resultant nomogram was internally validated and had a concordance index c of 0.69. c = 1 indicates perfect prediction accuracy and c = 0.5 is as good as a random predictor.
This study was concluded pre- PSMA Pet scan which would close the gap mentioned wherein sRT was provided to men with MET. Before any sRT is given today a PSMA Pet scan would be needed and should be SOC (standard of care) in order to determine if MET is present. In this case sRT is not an option. Should this study be replicated and patients failing the PSMA Pet are excluded, it would or should increase the c, or concordance index, appropriately.
For me, 9 months after the start of my ADT holiday, with a nadir of 0.001 ng/dL and 3 each uPSA (ultra low PSA) test results, my total now stands at 156. This means that I have a 57% chance of being PFP at 6 years post sRT...that would take me to 2026...time will tell. The 57% from the nomogram tracks other predictive models I have used, which range from a low of 50% upwards.
Details;
1. Median Time to MET - An estimated 25% of patients treated with radical prostatectomy (RP) for clinically localized prostate cancer will suffer recurrence of their disease. In the absence of salvage therapy (sRT), the median time from PSA recurrence to distant metastasis is 8 years.
2. Primary End Points – For this study they were;
a. disease progression after SRT, defined as a serum PSA value of 0.2 ng/mL or more above the postradiotherapy nadir followed by another higher value,
b. a continued rise in the serum PSA despite SRT,
c. initiation of systemic therapy after completion of SRT, or
d. clinical progression.
3. 6 Year Response from sRT - The 6-year response to SRT among patients treated at PSA levels of 0.50 ng/mL or less appears to be durable because only two progression events were observed after 6 years among 32 patients at risk at 6 years (error in Fig 1 which shows 11 at Risk for month 90; should be 30). 1,491 patients and their responses to sRT were available. For these;
a. a PSA nadir after radiotherapy of 0.10 ng/mL or less was achieved in 905 patients,
b. 726 patients did not receive ADT.
c. 600 patients received ADT.
4. Risk Subsequent PSA Progression - patients who experienced two or more PSA rises at levels of 0.2 ng/mL or higher or a single PSA level of 0.5 ng/mL or higher, are associated with a risk of subsequent PSA progression that is greater than 90%.
5. Efficacy of ADT Treatment - ADT administered before and/or during SRT was associated with improved PSA control in the study, although this may potentially be explained by the effects of prolonged ADT (up to 24 months in some patients) on masking PSA recurrence.
6. Use of Nomogram - The nomogram represents the best tool available (circa 2009; pre PSMA PET) to predict the outcome of SRT and is anticipated to be useful for medical decision making for patients with a rising PSA.