I have had 21 months of ADT and also have decided to stop short of my suggested 24 months total treatment as of December, 2022; I cant take the low TET anymore and its consequent impacts. Just when I was doubting my choice to move to long term ADT (LTADT) after salvage radiation (sRT) I stumbled on this study which I had looked at some months back; it gives me pause...
I have counseled here against haphazard, or reflexive use of ADT; it has significant side effects and for ED deals a terminal blow to restoring natural erectile function...but this enormous study of 21,429 men begs to differ with my newfound remorse and reminded me that I made the right call, at the right time, for the condition I had. With a whopping Decipher score of 0.97 (1.0 is the maximum score) I had a lethal PCa cell type and having recurrent PSA of 0.13 at 6 weeks post surgery I had to move fast and aggressively. Now reading the results of this prospective study I am glad I did...
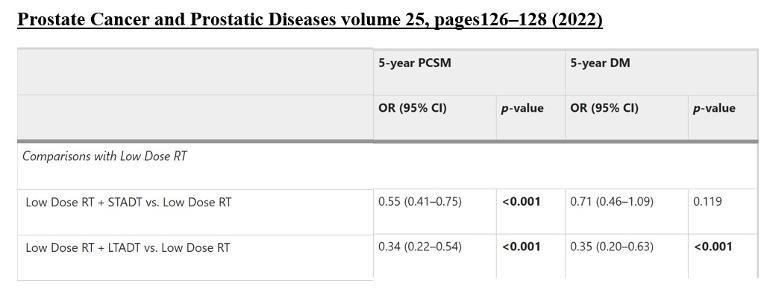
Read my take-away from the study and find the link to do your own analysis. The bottom line is that the OR (odds ratios) against 5 year PCSM improved between using LTADT with low dose RT (radiation therapy) vs low dose RT alone; 66% survival vs 34% mortality...this is at 5 years. At 10 years the benefit continues with an OR improvement against PCSM rising from 52% to 71% between ST and LTADT + low dose RT. Most of these OR's had 'p factors' of 0.001, or 1 tenth of a percent ( 0.10%), that the result was null (wrong)...very low odds. See the link below that explain OR's.
I am aware that this is all a numbers game, but all we can use to make informed decisions are the OR's and 'p factors' that come out of medical studies. Otherwise we move forward with treatment ignorant of why we choose one regime over another, or we put ourselves at the mercy of our Doctors who are very busy professionals not meaning to do wrong, but who occasionally don’t pay close attention to calibrating treatments to specific conditions (that is as much British understatement as I can muster).
See if this study helps you make informed decisions. I stand by my conclusion that ADT should never be used until and unless its absolutely needed; never as a universal prophylactic. BUT if you need it, use it! It will give you a significant increased chance of survival, protection from metastasis and a chance to complain about it later...Rick
PS one disturbing aspect of using ADT with radiation treatment appears to be the production of PCa cells which become 'radiation resistant,' evil twins of their castrate resistant, androgen independent cousins. Check out the call out for footnote 7...reminds me that PCa treatment is a human version of 'Wacka-Mole,' that great Chuckie Cheese game where regardless how good you are you cant seem to get ahead...but I will go with the numbers and stick to my decision for my particular case...
Prostate Cancer and Prostatic Diseases volume 25, pages126–128 (2022)
Background: Trials have included treatment strategies that incorporate either high or low dose RT (Radiaiton Therapy less than 72 Gy), or short-term or long-term ADT (STADT 18mo), in one or more trial arms. We sought to compare different forms of treatment intensification of RT in the context of localized prostate cancer and use of ADT in both STADT and LTADT.
Results: Dose-escalation either in the absence or presence of STADT failed to significantly improve any 5-year outcome. In contrast, adding LTADT to low dose RT significantly improved 5-year PCSM (Odds ratio [OR] 0.34, 95% confidence interval [CI] 0.22–0.54, p < 0.001) and DM (OR 0.35, 95% CI 0.20–0.63. p < 0.001) over low dose RT alone. Adding STADT also significantly improved 5-year PCSM over low dose RT alone (OR 0.55, 95% CI 0.41–0.75, p < 0.001).
Conclusions: Adding ADT, versus increasing RT dose alone, offers a more consistent improvement in clinical endpoints.
Method: A meta-regression of 40 individual trials with 21,429 total patients to allow a comparison of the rates and cumulative proportions of 5-year overall survival (OS), prostate cancer-specific mortality (PCSM), and distant metastasis (DM) for each treatment arm of every trial. Strategies were as follows;
a. low dose RT alone (n = 5401 patients from 15 trials),
b. high dose RT alone (n = 5009 patients from 11 trials),
c. low dose RT + short-term ADT (STADT, n = 6482 from 11 trials),
d. low dose RT + long-term ADT (LTADT, n = 2760 patients from 6 trials), and
e. high dose RT + STADT (n = 1777 patients from 5 trials).
f. high dose RT + LTADT (not done)
Discussion:
a. Doses higher than 74 Gy were considered “high dose” (presuming an α/β of 3.0 to convert hypofractionated schedules),
b. STADT was defined as ≤8 months
c. LTADT was defined as ≥18 months (Table 1)
d. The null hypothesis was rejected at P < 0.006 for OS and PCSM or P < 0.008 level for DM
e. The median follow-up for all trial arms was 9.15 years.
f. There was no significant difference in 10 year outcomes for PCSM, or DM when comparing high dose RT alone or low dose RT alone, without STADT.
g. When considering low dose RT + STADT as the reference group, prolongation to LTADT improved 5-year DM (OR 0.50, 95% CI 0.30–0.81). 50% chance for DM.
h. Low dose RT + LTADT showed statistical improvement in 10-year PCSM when compared to low dose RT + STADT (OR 0.29 vs 0.58, 95% CI, p=0.001; Table 4), a 71% chance of survival vs 52%, or a 19% improvement.
i. Escalating RT dose in the absence of ADT demonstrated no significant improvement in OS, PCSM, or DM, and appeared to be associated with worse outcomes compared to low dose RT + LTADT.
j. Notably, as a radiosensitizer, ADT increases local control, but can also have cytostatic, if not cytocidal, effects on micrometastatic disease [7].
• Ref (7) abstract; ADT during RT can promote cancer cell radiotherapy resistance
• We establish that prostate cancer cells treated with ionizing radiation plus androgen demonstrate enhanced DNA repair and decreased DNA damage and furthermore that
• Antiandrogen treatment causes increased DNA damage and decreased clonogenic survival.
• Our data establish that AR signaling increases the expression of DNA repair genes and, in parallel,
• Promotes prostate cancer radioresistance by accelerating repair of ionizing radiation–induced DNA damage.
Definitions:
a. OR Odds Ratio - the odds of an event is the number of those who experience the event divided by the number of those who do not.
b. p Value - If the p-value is equal to or less than a predetermined cutoff (usually 0.05, or a 5 in 100 probability that the finding is due to chance alone), the association is said to be statistically significant. If it is greater than the predetermined cutoff, the association is said to be not statistically significant.
c. STADT - Short term ADT treatment of less than 18 months
d. LTADT - Long term ADT treatment of greater than 18 months
e. ADT - Androgen deprivation treatment
f. PCSM - prostate cancer-specific mortality
g. OS - overall survival
h. DM - distant metastasis
i. AR - androgen receptor
References:
nature.com/articles/s41391-...
Ref (7): cancerdiscovery.aacrjournal...
OR Ratio: youtu.be/rhrqDAEDNsM