For anyone thinking about Salvage Radiation Treatment (SRT) this article makes the point that you should have your PSA measured before, during (25th session) and after treatment...my Doctor did not believe this was necessary; I see now that it was. Luckily I had my own tests done at ultra low levels (uPSA) both before and immediately after my salvage, so I can 'plug' myself into the matrix of this test...but forewarned is forearmed...Cheers
Purpose: Determine whether a rising interim prostate-specific antigen (PSA) during radiation therapy can predict the likelihood of subsequent biochemical recurrence.
Summary:
- Techniques are needed to determine whether a patient has pelvis-confined recurrent disease
- A falling PSA during salvage postprostatectomy radiation therapy may be the earliest indication that a patient does have at least a component of residual disease in the prostate bed.
- Conversely, a rising PSA during salvage radiation therapy may suggest that a patient has disease beyond the radiation therapy field and therefore is destined to fail salvage prostate bed radiation therapy.
- A drop in PSA during during radiation therapy and a positive surgical margin were significant factors for freedom from subsequent biochemical failure (BCF), and
- All patients with a rising interim PSA, negative surgical margin, and seminal vesicle invasion ultimately had biochemical failure at 2 years.
Methods: between 2010 and 2016;
- 185 patients had salvage radiation therapy (RT) to a dose of 68 Gy without androgen deprivation therapy for a rising PSA level after radical prostatectomy.
- The median age was 66 years. Of the 185 patients, 63 (34.1%) had pT2 disease and 122 (65.9%) had pT3 disease.
a. 146 (78.9%) had a Gleason score of 7;
b. 33 (17.8%) had a Gleason score >7,
c. 6 (3.2%) had a Gleason score ≤6.
- A pelvic lymph node dissection was performed in 140 (75.7%) of patients; all patients were lymph node negative (N0),
- extra prostatic extension (EPE) w positive surgical margin was found in 112 (60.5%) of the patients.
- Patients received 68 Gy in 34 fractions (2 Gy per fraction, 5 fractions per week) using a 3-dimensional conformal external beam radiation therapy (EBRT) technique (2010-2014) or
- an intensity modulated radiation therapy (IMRT) /volumetric modulated arc therapy (VMAT) external beam radiation therapy technique. Daily cone beam computed tomography images with soft tissue matching was used.
- these patients did not receive ADT and did not have pelvic lymph nodes treated with radiation therapy.
- Patients had their PSA recorded on the first day of radiation therapy and again after completing the 25th fraction (of 34 total fractions).
- Biochemical failure (BCF) after radiation therapy was defined as a PSA value ≥0.2 ng/mL within 2 years after radiation therapy.
Results: for 185 patients;
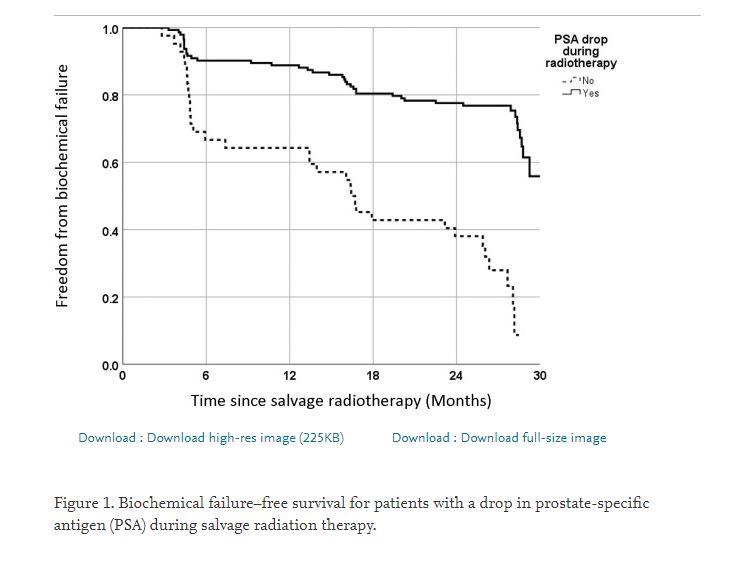
- The 2-year freedom from biochemical failure (BCF) was 60%
- For the interim PSA test (25th Fraction), 143 of 185 patients (77%) had a drop in PSA during RT;
a. of these 143 patients, 102 (71%) had 2-year biochemical control.
b. the balance of 42 patients (23%) had a stable or rising interim PSA, and
c. only 10 (24%) of these 42 patients had 2-year biochemical control.
Discussion:
- Approximately 30% of men with localized prostate cancer will develop detectable prostate-specific antigen (PSA) levels after a radical prostatectomy (RP), and
- 2/3 two-thirds of these men will develop metastatic prostate cancer if left untreated.
a. Salvage radiation therapy (RT) after a rise in PSA after a radical prostatectomy offers a second chance at a cure,
b. Salvage radiation therapy resulting in long-term biochemical control rates of approximately 50%.
c. prostate bed RT is a standard treatment for patients with a rising PSA after RP.
- PSMA PET scan at the time of biochemical relapse improves the chances of detecting macroscopic tumor compared with conventional imaging.
a. but, at ultralow PSA levels, macroscopic disease often cannot be detected.
b. with PSA values <0.2 ng/mL, detection rates with PSMA PET are only 33.3% (sensitivity).
c. most patients are considered for salvage postprostatectomy radiation therapy with a PSA level <0.2 ng/mL