I have received my blood tests can anyone advise me on them please.I take 50 mg levothyroxine each day, I did not take it the day before my blood test.
Thank you
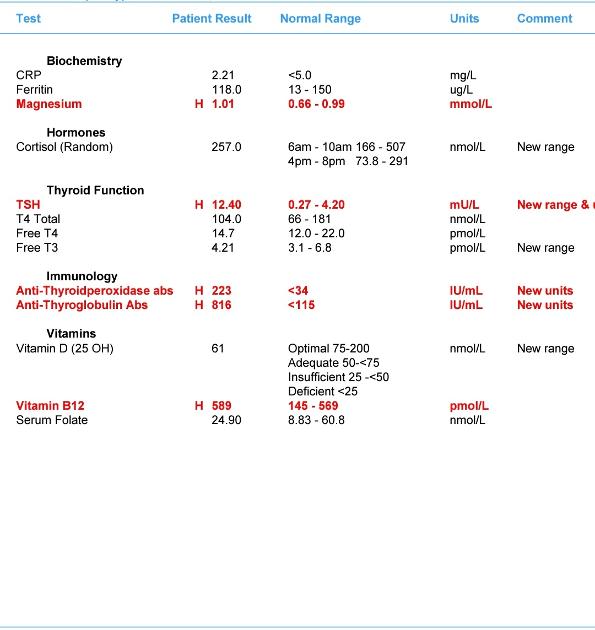
I have received my blood tests can anyone advise me on them please.I take 50 mg levothyroxine each day, I did not take it the day before my blood test.
Thank you
Dawney63
Your post of two weeks ago told us you'd just restarted Levo 4 weeks prior, so you've been back on Levo lat 50mcg daily for approx 6 weeks. Your TSH tested with your GP was 8.5 and now it's increased to 12.4
I'm wondering if you did both tests under the same conditions, ie
* No later than 9am
* Nothing to eat or drink but water before the test
* Last dose of Levo 24 hours before test
* No biotin, B Complex or any supplement containing biotin for 3-7 days before testing
If you followed the above testing protocol clearly your current TSH is way too high and FT4 way too low and you need an increase in your dose of Levo, 25mcg now and retest in 6-8 weeks, and I expect further increases will be required. The aim of a treated hypo patient on Levo only, generally, is for TSH to be 1 or below with FT4 and FT3 in the upper part of their reference ranges, if that is where you feel well.
Your raised antibodies confirm that the cause of your hypothyroidism is autoimmune, known to patients as Hashimoto's but usually called autoimmune thyroiditis or autoimmune thyroid disease by the medical profession.
Hashi's is where the immune system attacks and gradually destroys the thyroid resulting in hypothyroidism. Fluctuations in symptoms and test results are common with Hashi's.
Some members have found that adopting a strict gluten free diet can help, although there is no guarantee.
Gluten contains gliadin (a protein) which is thought to trigger autoimmune attacks so eliminating gluten can help reduce these attacks.
You don't need to be gluten sensitive or have Coeliac disease for a gluten free diet to help.
Gluten/thyroid connection: chriskresser.com/the-gluten...
stopthethyroidmadness.com/h...
stopthethyroidmadness.com/h...
hypothyroidmom.com/hashimot...
thyroiduk.org.uk/tuk/about_...
Supplementing with selenium l-selenomethionine 200mcg daily is said to help reduce the antibodies, as can keeping TSH suppressed.
Do you take any supplements at all? Your B12 is over range but your folate could be a bit better.
Continued below due to character restriction.
Hashi's and gut absorption problems tend to go hand in hand and can very often result in low nutrient levels or deficiencies.
Your Vit D could be a lot better. A level of 100-150nmol/L is recommended by the Vit D Council, Vit D Society and Grassroots Health, with a recent blog post on Grassroots Health recommending at least 125nmol/L.
You might want to check out a recent post that I wrote about Vit D and supplementing:
healthunlocked.com/thyroidu...
and you can check out the link to how to work out the dose you need to increase your current level to the recommended level.
Your current level of 61nmol/L = 24.4ng/ml
On the Vit D Council's website
web.archive.org/web/2019070...
you would scroll down to the 3rd table
My level is between20-30 ng/ml
So now you look at how much is needed to reach 50ng/ml (125nmol/L) and you'll see that they suggest 3,700iu per day, the nearest to buy is 4,000iu but it is cheaper to buy 5,000iu dose. 4,000 x 7 days = 28,000iu so you could take 5,000iu x 6 days = 30,000iu and that would be fine.
Retest after 3 months.
Once you've reached the recommended level then a maintenance dose will be needed to keep it there, which may be 2000iu daily, maybe more or less, maybe less in summer than winter, it's trial and error so it's recommended to retest once or twice a year to keep within the recommended range. This can be done with a private fingerprick blood spot test with an NHS lab which offers this test to the general public:
Doctors don't know, because they're not taught much about nutrients, but there are important cofactors needed when taking D3. You will have to buy these yourself.
D3 aids absorption of calcium from food and Vit K2-MK7 directs the calcium to bones and teeth where it is needed and away from arteries and soft tissues where it can be deposited and cause problems such as hardening of the arteries, kidney stones, etc. 90-100mcg K2-MK7 is enough for up to 10,000iu D3.
D3 and K2 are fat soluble so should be taken with the fattiest meal of the day, D3 four hours away from thyroid meds if taking D3 as tablets/capsules/softgels, no necessity if using an oral spray.
For D3 I like Doctor's Best D3 softgels, they are an oil based very small softgel which contains just two ingredients - D3 and extra virgin olive oil, a good quality, nice clean supplement which is budget friendly. Some people like BetterYou oral spray but this contains a lot of excipients and works out more expensive.
For Vit K2-MK7 my suggestions are Vitabay, Vegavero or Vitamaze brands which all contain the correct form of K2-MK7 - the "All Trans" form rather than the "Cis" form. The All Trans form is the bioactive form, a bit like methylfolate is the bioactive form of folic acid.
Vitabay and Vegavero are either tablets or capsules.
Vitabay does do an oil based liquid.
Vitamaze is an oil based liquid.
With the oil based liquids the are xx amount of K2-MK7 per drop so you just take the appropriate amount of drops.
They are all imported German brands, you can find them on Amazon although they do go out of stock from time to time. I get what I can when I need to restock. If the tablet or capsule form is only in 200mcg dose at the time I take those on alternate days.
Another "all trans" one worth considering if the others aren't availaable:
amazon.co.uk/Vitality-Biore...?
If looking for a combined D3/K2 supplement, this one has 3,000iu D3 and 50mcg K2-MK7. The K2-MK7 is the All-Trans form
natureprovides.com/products...
It may also be available on Amazon.
One member recently gave excellent feedback on this particular product here:
Here is what she said (also read the following replies):
healthunlocked.com/thyroidu...
Another important cofactor is Magnesium which helps the body convert D3 into it's usable form.
There are many types of magnesium so we have to check to see which one is most suitable for our own needs:
naturalnews.com/046401_magn...
explore.globalhealing.com/t...
and ignore the fact that this is a supplement company, the information is relevant:
swansonvitamins.com/blog/ar...
Magnesium should be taken 4 hours away from thyroid meds and as it tends to be calming it's best taken in the evening. Vit D should also be taken 4 hours away from thyroid meds. Vit K2-MK7 should be taken 2 hours away from thyroid meds. Don't take D3 and K2 at the same time unless both are oil based supplements, they both are fat soluble vitamins which require their own fat to be absorbed otherwise they will compete for the fat.
Don't start all supplements at once. Start with one, give it a week or two and if no adverse reaction then add the next one. Again, wait a week or two and if no adverse reaction add the next one. Continue like this. If you do have any adverse reaction then you will know what caused it.
So GP should increase dose levothyroxine to 75mcg
Which brand of levothyroxine are you currently taking
Retest thyroid levels again 6-8 weeks after increasing dose
Likely to need further increase after that
The blood test I had done private was taken at 9am, I stopped all vitamin supplements a week before , i had been taking menopace plus (thought my issues might have been related to the menopause) .I hadn't had anything to eat before the test and stopped my levothyroxine the day before.
My antibodies have been high for a few years now and my GP woukd say at some point your thyroid will go underactive.
It was overactive 1983-1987
My mum and sister both had underactive.
Not sure which levothyroxine the box says Almus on it.
Thank you for the advice.
Almus has Accord brand inside
Accord don’t make 25mcg tablets
Request GP increase number of 50mcg tablets prescribed per month and cut a 50mcg in half to get 25mcg daily
Many people find Levothyroxine brands are not interchangeable.
Most easily available (and often most easily tolerated) are Mercury Pharma or Accord
Mercury Pharma make 25mcg, 50mcg and 100mcg tablets
Mercury Pharma also boxed as Eltroxin. Both often listed by company name on pharmacy database - Advanz
Accord only make 50mcg and 100mcg tablets
Accord is also boxed as Almus via Boots,
Many patients do NOT get on well with Teva brand of Levothyroxine. Teva is lactose free.
But Teva contains mannitol as a filler instead of lactose, which seems to be possible cause of problems. Mannitol seems to upset many people, it changes gut biome
Teva is the only brand that makes 75mcg tablet.
So if avoiding Teva for 75mcg dose ask for 25mcg to add to 50mcg or just extra 50mcg tablets to cut in half
But for some people (usually if lactose intolerant, Teva is by far the best option)
Aristo (currently 100mcg only) is lactose free and mannitol free.
March 2023 - Aristo now called Vencamil
healthunlocked.com/thyroidu...
Wockhardt is very well tolerated, but only available in 25mcg tablets. Some people remain on Wockhardt, taking their daily dose as a number of tablets
List of different brands available in U.K.
thyroiduk.org/if-you-are-hy...
Posts that mention Teva
healthunlocked.com/search/p...
Teva poll
healthunlocked.com/thyroidu...
Once you find a brand that suits you, best to make sure to only get that one at each prescription.
Watch out for brand change when dose is increased or at repeat prescription.
Government guidelines for GP in support of patients if you find it difficult/impossible to change brands
gov.uk/drug-safety-update/l...
If a patient reports persistent symptoms when switching between different levothyroxine tablet formulations, consider consistently prescribing a specific product known to be well tolerated by the patient.
academic.oup.com/jcem/artic...
Physicians should: 1) alert patients that preparations may be switched at the pharmacy; 2) encourage patients to ask to remain on the same preparation at every pharmacy refill; and 3) make sure patients understand the need to have their TSH retested and the potential for dosing readjusted every time their LT4 preparation is switched (18).
Have you had coeliac blood test done
Or are you already on strictly gluten free diet
Your antibodies are high this is Hashimoto's, (also known by medics here in UK more commonly as autoimmune thyroid disease).
Hashimoto's affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances. Most common by far is gluten. Dairy is second most common.
A trial of strictly gluten free diet is always worth doing
Only 5% of Hashimoto’s patients test positive for coeliac but a further 81% of Hashimoto’s patients who try gluten free diet find noticeable or significant improvement or find it’s essential
A strictly gluten free diet helps or is essential due to gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and may slowly lower TPO antibodies
While still eating high gluten diet ask GP for coeliac blood test first or buy test online for under £20, just to rule it out first
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
pubmed.ncbi.nlm.nih.gov/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
Similarly few months later consider trying dairy free too. Approx 50-60% find dairy free beneficial
Hashimoto’s and leaky gut often occur together
I'm not on a gluten free diet will get a test done for coliac.Have lots of heartburn on lanzoprole.
As dose levothyroxine is increased up you should be able to reduce and stop Lansoprazole
Are you taking this at least 4 hours away from levothyroxine
Most hypothyroid patients have LOW stomach acid
Frequently misdiagnosed as high acid
Lansoprazole (a PPI) is to treat high stomach acid
Virtually identical symptoms, but very different treatment
However you can not just stop any PPI …have to ween off slowly……when on higher dose levothyroxine and thyroid levels are improving
Low stomach acid can be a common hypothyroid issue
Thousands of posts on here about low stomach acid
healthunlocked.com/search/p...
Web links re low stomach acid and reflux and hypothyroidism
nutritionjersey.com/high-or...
stopthethyroidmadness.com/s...
thyroidpharmacist.com/artic...
How to test your stomach acid levels
healthygut.com/articles/3-t...
meraki-nutrition.co.uk/indi...
huffingtonpost.co.uk/laura-...
lispine.com/blog/10-telling...
Useful post and recipe book
healthunlocked.com/thyroidu...
Protect your teeth if using ACV with mother
healthunlocked.com/thyroidu...
Ppi
Omeprazole or Lansoprazole will tend to lower vitamin levels even further
gov.uk/drug-safety-update/p...
webmd.com/heartburn-gerd/ne...
pharmacytimes.com/publicati...
PPI and increased risk T2 diabetes
gut.bmj.com/content/early/2...
Iron Deficiency and PPI
medpagetoday.com/resource-c...
futurity.org/anemia-proton-...
onlinelibrary.wiley.com/doi...
sciencedirect.com/science/a...
But never assume you have low stomach acid and never stop Lansoprazole suddenly
healthygut.com/4-common-bet...
Thank you, I'm trying to put all the pieces together , last October GP put me on a 3 month course of folic acid due to low folate levels.The ringing in my ears/head, reflux, tiredness, lack of motivation, weight gain can all be caused by my thyroid issues?
yes absolutely
Symptoms of hypothyroidism
thyroiduk.org/wp-content/up...
Most common symptoms are weight gain, depression/anxiety, poor digestion/IBS/bloating (due to low stomach acid), fatigue
Low stomach acid results in poor nutrient absorption and low vitamin levels as direct result
What vitamin supplements are you now taking
Presumably you have finished folic acid prescription
Suggest you start supplementing a good quality daily vitamin B complex, one with folate in (not folic acid)
This can help keep all B vitamins in balance
Difference between folate and folic acid
healthline.com/nutrition/fo...
Many Hashimoto’s patients have MTHFR gene variation and can have trouble processing folic acid.
thyroidpharmacist.com/artic...
B vitamins best taken after breakfast
Thorne Basic B recommended vitamin B complex that contains folate, but they are large capsules. (You can tip powder out if can’t swallow capsule)
Thorne currently difficult to find at reasonable price, should be around £20-£25. iherb.com often have in stock. Or try ebay
Other options
healthunlocked.com/thyroidu....
IMPORTANT......If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 7 days before ALL BLOOD TESTS , as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
In week before blood test, when you stop vitamin B complex, you might want to consider taking a separate folate supplement (eg Jarrow methyl folate 400mcg) and continue separate B12
Also improving low vitamin D to at least around 80nmol-100nmol
I didn't take the folic acid tablets the GP prescribed I took solgar folate 1000, I use a magnesium spray (not every day when I get cramps in my legs) should I use it every day ?I have ordered D3/K2 drops
So I also need a B complex vitamin the one you suggest if you tip the powder out do you put it in food or a drink ? (I can't swallow big tablets)
Im on high blood pressure tablets and statins prescribed by GP.
Should I ask GP to be referred to a consultant at hospital?
Thank you.
High blood pressure should improve as thyroid levels improve
High cholesterol is symptom of hypothyroidism
nhs.uk/conditions/statins/c...
If you have an underactive thyroid (hypothyroidism), treatment may be delayed until this problem is treated. This is because having an underactive thyroid can lead to an increased cholesterol level, and treating hypothyroidism may cause your cholesterol level to decrease, without the need for statins. Statins are also more likely to cause muscle damage in people with an underactive thyroid.
just to clarify .. you said you didn't take levo the day before the test ?
if you usually take your levo in the morning, then you should take levo as usual the day before the test .
On the morning of the test , don't take that day's dose until after the test (you want approx 24 hr gap from last dose )
Doctor will need to do their own blood test, that is usual.... they won't usually accept private results .
Thats correct I didn't take levo the day before the test.I am feeling quiet unwell the last 2 days.
I use a fit bit watch not sure how accurate they are but resting heart rate is always in 50's don't know if this is significant in any way to thyroid problems
Hi Dawney, i'm not surprised you feel unwell with TSH so high , it is a clear signal that you are hypothyroid and your body wants a higher dose of Levo.
So , organise the retest at GP as soon as possible .
GP should then increase dose to 75mcg.
in future test DO NOT miss levo the day before the test (leaving longer than 24hrs gives a false low fT4 result)
Just delay taking the dose that's due ON THE MORNING OF THE TEST and take it afterwards. (you don't want to test within about 12 hrs of taking levo as that gives a false high fT4 result)
Preferably get an early A.M blood draw , 9 am ish and try to get all future blood draws at the same time of day (TSH is naturally higher in early am and falls throughout the day till its lowest around 1-3pm .. so you want to do all tests at similar time so TSH results can be compared accurately to previous ones)
You should hopefully start to feel a bit better once you've been taking 75mcg for week or two., and yes a slow heart rate is a symptom of being hypothyroid, this should improve once you are on higher doses.
6 -8 weeks after you've started on 75mcg , organise another retest with GP .. it is quite likely that you will need a further increase in levo at that point , most people end up on somewhere between 75- 150mcg (even if TSH is 'in range' on 75mcg and GP say's 'that's ok now' , it may not be 'optimal' for you .. many people don't feel properly well until TSH is around 1 ish, and some need it lower than that .... explanation here : healthunlocked.com/thyroidu... the-shoe-size-analogy.-* )
Come back to us with results after 6-8 weeks on 75mcg to let us know how you're doing.
Thank youI arranged a blood test for next Thursday at 9.45am, I can get a cancellation tomorrow at 7.45am woukd 7.45am be ok? Or should I wait for next Thursday at 9.45am ?.
I take my levo about 7am so I should take day before but not take on the day of blood test?
Sorry for all ?s but I get so anxiouse I will do.it wrong.