My son 28 was diagnosed with hashinotos in 2016 and given levothyroxine...consultant took him off levo 2 years ago ...advising GP to reinstate when TSH gets to 10 ...surely he needs levo now ...his bloods look awful and he feels really unwell ...off sick with low mood and anxiety ...has a follow-up with gp Tuesday to discuss and I would appreciate any advice..I've read recently that untreated hypothyroidism can lead to non alcoholic fatty liver disease particularly in men. Could this be happening here ?
Recent blood results : My son 28 was diagnosed... - Thyroid UK
Recent blood results
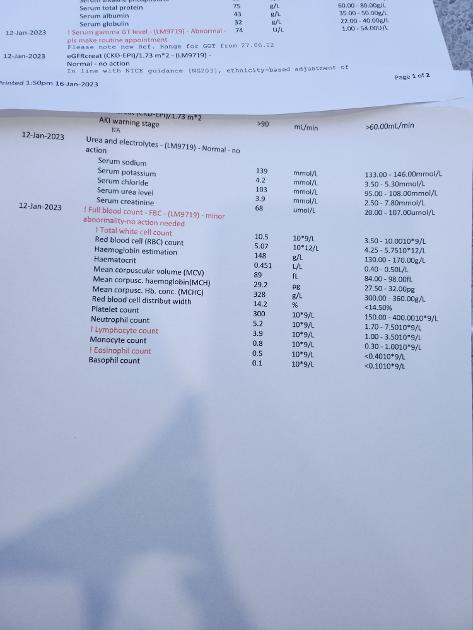
There’s no thyroid or relevant vitamin results here
Sounds like endocrinologist was diabetes specialist
With Hashimoto’s and symptoms if TSH is over 5 should be prescribed levothyroxine
Once on levothyroxine levothyroxine should be increased slowly upwards in 25mcg steps until TSH is ALWAYS below 2
Most people when adequately treated will have Ft4 and Ft3 at least 70% through range and frequently TSH will be around or under one
For full Thyroid evaluation your son need TSH, FT4 and FT3 tested
You already know he has Hashimoto’s
Very important to test vitamin D, folate, ferritin and B12 at least once year minimum
Having had levothyroxine stopped he likely has terrible vitamin levels
Recommended on here that all thyroid blood tests early morning, ideally just before 9am
(and once back on levothyroxine….last dose levothyroxine 24 hours before test )
This gives highest TSH, lowest FT4 and most consistent results. (Patient to patient tip)
Private tests are available as NHS currently rarely tests Ft3 or all relevant vitamins
List of private testing options and money off codes
thyroiduk.org/getting-a-dia...
Medichecks Thyroid plus antibodies and vitamins
medichecks.com/products/adv...
Blue Horizon Thyroid Premium Gold includes antibodies, cortisol and vitamins
bluehorizonbloodtests.co.uk...
If you can get GP to test vitamins then cheapest option for just TSH, FT4 and FT3
£29 (via NHS private service ) and 10% off down to £26.10 if go on thyroid uk for code
thyroiduk.org/getting-a-dia...
Monitor My Health also now offer thyroid and vitamin testing, plus cholesterol and HBA1C for £65
(Doesn’t include thyroid antibodies)
monitormyhealth.org.uk/full...
10% off code here
thyroiduk.org/getting-a-dia...
NHS easy postal kit vitamin D test £29 via
Only do private testing early Monday or Tuesday morning.
Watch out for postal strikes, probably want to pay for guaranteed 24 hours delivery
Link about thyroid blood tests
thyroiduk.org/getting-a-dia...
Link about Hashimoto’s
thyroiduk.org/hypothyroid-b...
Symptoms of hypothyroidism
thyroiduk.org/wp-content/up...
Page 2 was missing from picture which shows some vit tests and tsh his vit D is 7
make urgent appointment with GP
Folate is severely deficient
B12 is severely deficient
Vitamin D is severely deficient
TSH over 5 confirms he must be started on levothyroxine
Standard starter dose of levothyroxine is 50mcg
Bloods should be retested 6-8 weeks after each dose increase
ALWAYS book early morning test at around 9am and last dose levothyroxine 24 hours before test
Meanwhile ESSENTIAL To be improving low vitamin levels
Can’t see any iron/ferritin test results
He needs full iron panel test for anaemia including ferritin
And coeliac blood test
All this is DIRECT RESULT of endocrinologist inappropriately stopping levothyroxine
standard starter dose of levothyroxine is 50mcg
Dose is increased slowly upwards in 25mcg steps until on approx 1.6mcg levothyroxine per kilo per day
Many people find different brands of levothyroxine are not interchangeable
Once he works out which brand suits best …..try to always get same brand
pathlabs.rlbuht.nhs.uk/tft_...
Guiding Treatment with Thyroxine:
In the majority of patients 50-100 μg thyroxine can be used as the starting dose. Alterations in dose are achieved by using 25-50 μg increments and adequacy of the new dose can be confirmed by repeat measurement of TSH after 2-3 months.
The majority of patients will be clinically euthyroid with a ‘normal’ TSH and having thyroxine replacement in the range 75-150 μg/day (1.6ug/Kg on average).
The recommended approach is to titrate thyroxine therapy against the TSH concentration whilst assessing clinical well-being. The target is a serum TSH within the reference range.
……The primary target of thyroxine replacement therapy is to make the patient feel well and to achieve a serum TSH that is within the reference range. The corresponding FT4 will be within or slightly above its reference range.
The minimum period to achieve stable concentrations after a change in dose of thyroxine is two months and thyroid function tests should not normally be requested before this period has elapsed.
Starting levothyroxine - flow chart
NHS N.I.C.E guidelines for thyroid disease diagnosis and treatment: say patient CAN be started on Levo BEFORE TSH gets to 10 under some circumstances ~ if symptoms of hypothyroidism are an issue, he could be started on levothyrxoine when TSH is "over range but under 10" on two occasions 3 months apart . and raised TPOab (previous Hashimoto's diagnosis) should be taken into account , in the decision to treat before TSH gets to 10.
(*note ~ 'subclinical hypothyroidism' means "TSH is over reference range ,while fT4 is still within range")
"1.5 Managing and monitoring subclinical hypothyroidism
Tests for people with confirmed subclinical hypothyroidism
Adults
1.5.1Consider measuring TPOAbs for adults with TSH levels above the reference range, but do not repeat TPOAbs testing.
Treating subclinical hypothyroidism
1.5.2When discussing whether or not to start treatment for subclinical hypothyroidism, take into account features that might suggest underlying thyroid disease, such as symptoms of hypothyroidism, previous radioactive iodine treatment or thyroid surgery, or raised levels of thyroid autoantibodies.
Adults
1.5.3Consider levothyroxine for adults with subclinical hypothyroidism who have a TSH of 10 mlU/litre or higher on 2 separate occasions 3 months apart. Follow the recommendations in section 1.4 on follow-up and monitoring of hypothyroidism.
1.5.4Consider a 6-month trial of levothyroxine for adults under 65 with subclinical hypothyroidism who have:
a TSH above the reference range but lower than 10 mlU/litre on 2 separate occasions 3 months apart, and
symptoms of hypothyroidism.
If symptoms do not improve after starting levothyroxine, re-measure TSH and if the level remains raised, adjust the dose. If symptoms persist when serum TSH is within the reference range, consider stopping levothyroxine and follow the recommendations on monitoring untreated subclinical hypothyroidism and monitoring after stopping treatment."
I don't know if any of his other 'out of range' results are relevant to this, but i will add it incase it's helpful:
NHS N.I.C.E Clinical knowledge Summary
cks.nice.org.uk/topics/hypo...
Complications of untreated or undertreated hypothyroidism include:
Impaired quality of life due to symptoms such as fatigue.
Cardiovascular
Dyslipidaemia [Chaker, 2017]
Several studies, including a large epidemiological survey (n = 25,862), have identified a relationship between increased thyroid-stimulating hormone (TSH) and dyslipidaemia [Canaris et al, 2000; Pearce, 2013].
Metabolic syndrome [Chaker, 2017]
Hypothyroidism is associated with a decrease in insulin sensitivity, including direct effects on insulin secretion and clearance, leading to potential insulin resistance and increased risk of developing metabolic syndrome [Pearce, 2013].
Coronary heart disease (CHD) and stroke
A large meta-analysis including over 50,000 people from 11 prospective cohort studies found a statistically significant association between CHD mortality at TSH levels greater than 7 mU/L, and for cardiovascular events at TSH levels greater than 10 mU/L [Rodondi et al, 2010].
Epidemiological studies have shown an association between subclinical hypothyroidism and CHD in people younger than 65 years of age, and in those with TSH levels higher than 10 mU/L [Pearce, 2013; Okosieme, 2015; Bekkering, 2019]. The European Thyroid Association (ETA) guideline notes that the evidence regarding subclinical hypothyroidism and CHD events and mortality in the literature is conflicting [Pearce, 2013].
A large meta-analysis of 55 cohort studies (n = 1,898,314) found that people with hypothyroidism, compared with euthyroid controls, had higher risks of ischaemic heart disease (relative risk [RR] 1.13), myocardial infarction (RR 1.15), cardiac mortality (RR 1.96), and all-cause mortality (RR 1.25). A diagnosis of SCH was also associated with an increased risk of ischaemic heart disease and all-cause mortality. It found no significant association between hypothyroidism and risk of stroke, heart failure, or atrial fibrillation [Ning, 2017].
A retrospective cohort study of general practice patients with a diagnosis of hypothyroidism (n = 160,439) with a median follow-up of six years, found an increased risk of ischaemic heart disease and heart failure in people with high TSH concentrations (greater than 10 mU/L), with a hazard ratio of 1.18 and 1.42 respectively. In addition, increased all-cause mortality was observed with a hazard ratio of 2.21 [Thayakaran, 2019].
Heart failure
Untreated overt hypothyroidism has been associated with an increased risk of diastolic heart failure [Biondi, 2012; Chaker, 2017].
Subclinical hypothyroidism may be an independent risk factor for the development of heart failure and for progression of existing heart failure [Pearce, 2013; Chaker, 2017].
Neurological and cognitive
Overt hypothyroidism is associated with:
Decreased taste, vision, or hearing [Chaker, 2017].
Impaired attention, concentration, memory, language, executive function, and psychomotor speed [Gaitonde et al, 2012; Chaker, 2017].
Data on the association between subclinical hypothyroidism and cognitive impairment are inconsistent [Biondi, 2019].
One systematic review and meta-analysis of 15 studies (n = 19,944) found no evidence of an association between subclinical hypothyroidism and cognitive impairment in adults over 60 years of age [Akintola, 2015].
A meta-analysis of 15 studies on the association between subclinical hypothyroidism and depression (n = 12,315) found that people with subclinical hypothyroidism had a higher risk of depression than euthyroid controls (relative risk 2.35), and this was particularly marked in the older population cohort [Loh, 2019]."
cks.nice.org.uk/topics/hypo...
Management of subclinical hypothyroidism
"Consider offering a 6-month trial of LT4 monotherapy in adults less than 65 years of age if:
The TSH level is above the reference range but lower than 10 mU/L and FT4 is within the reference range on 2 separate occasions 3 months apart, and
There are symptoms of hypothyroidism.
If symptoms do not improve after starting LT4 therapy, measure the TSH level and if it remains raised, adjust the dose of LT4. Once the TSH level is stable (2 similar measurements within the reference range 3 months apart), check TSH annually.
If symptoms persist when the TSH is within the reference range, consider stopping LT4 therapy, and assess for alternative causes of symptoms.
Recheck serum lipids if needed, to see if they have improved or whether management for dyslipidaemia is needed. See the CKS topics on CVD risk assessment and management and Lipid modification - CVD prevention for more information."
Just back from doctors...shes refused to put him back on thyroxine or give him B12 supplements because she says they are all normal and she can't override the consultant and must wait for a TSH of 10.. basically sent him away with advice on alcohol use coz his liver enzymes are raised ..I'm so angry 😠
That's not on ... push back . ( tricky when it's not actually you ,and son is adult .. but try anyway)
put the references/ and request for levo in writing for the attention of Dr whatsit . maybe send a copy to the practice manager too while your at it , and say you've done this in your letter to Dr whatsit.
Since she's effectively 'copped out' of using the NIICE guidleines by passing the buck back to the endo saying 'he's in charge of this case' ...request she ACTUALLY contacts the endo now and informs him of the CURRENT symptoms and the urgency re. inability to work due to them.
The endos' instructions to her were made when you son was feeling well ... the situation has changed .. he is now very symptomatic , and so obviously if the endo IS still in charge of his care , then the endo needs to be updated , so he can tell her if his advice re '10' still stands in these changed circumstances ( since she appears not to be able to use her own brain or autonomy to help your son )
Also put something about requiring a response by 'x' date with an explanation IN WRITING of her refusal to follow NICE guideline re" 2 x TSh over range + symptoms + antibodies = consider levo" in your sons case.
Hope that is some use .. hopefully others will chime in with idea' s of 'what now'
Low vitamin D
GP should prescribe LOADING dose vitamin D
That’s 300,000iu over 6-8 weeks
And retest vitamin D levels at end of the course
NHS Guidelines on dose vitamin D required
ouh.nhs.uk/osteoporosis/use...
He will require ongoing daily vitamin D everyday
GP will often only prescribe to bring vitamin D levels to 50nmol.
Some areas will prescribe to bring levels to 75nmol or even 80nmol
leedsformulary.nhs.uk/docs/...
GP should advise on self supplementing if over 50nmol, but under 75nmol (but they rarely do)
mm.wirral.nhs.uk/document_u...
But with Hashimoto’s, improving to around 80nmol or 100nmol by self supplementing may be better
pubmed.ncbi.nlm.nih.gov/218...
vitamindsociety.org/pdf/Vit...
Test twice yearly via NHS private testing service when supplementing
Vitamin D mouth spray by Better You is very effective as it avoids poor gut function.
There’s a version made that also contains vitamin K2 Mk7.
One spray = 1000iu
amazon.co.uk/BetterYou-Dlux...
Another member recommended this one recently
Vitamin D with k2
amazon.co.uk/Strength-Subli...
It’s trial and error what dose we need, with thyroid issues we frequently need higher dose than average
Vitamin D and thyroid disease
grassrootshealth.net/blog/t...
Vitamin D may prevent Autoimmune disease
newscientist.com/article/23...
Web links about taking important cofactors - magnesium and Vit K2-MK7
Magnesium best taken in the afternoon or evening, but must be four hours away from levothyroxine
betterbones.com/bone-nutrit...
medicalnewstoday.com/articl...
livescience.com/61866-magne...
sciencedaily.com/releases/2...
Interesting article by Dr Malcolm Kendrick on magnesium
drmalcolmkendrick.org/categ...
Vitamin K2 mk7
B12 deficiency
His B12 is so low he will definitely need B12 injections
Typical to start with several B12 injections over 1-3 weeks….this is called LOADING B12
GP should test for Pernicious Anaemia before starting injections
Is your son vegetarian or vegan ?
No doubt he has plenty of Low B12 symptoms
b12deficiency.info/signs-an...
methyl-life.com/blogs/defic...
wether he then continues with injections every 1-3 months or changes to daily B12 supplements depends on GP and local policies
Daily B12 supplements
B12 drops
healthunlocked.com/thyroidu...
or
B12 sublingual lozenges
amazon.co.uk/Jarrow-Methylc...
cytoplan.co.uk/shop-by-prod...
B12 range in U.K. is too wide
Interesting that in this research B12 below 400 is considered inadequate
healthunlocked.com/thyroidu...
Note that improving folate when B12 is very low is not a good idea. Taking folate before B12 is good enough can lead to severe neurological problems.
en.wikipedia.org/wiki/Subac...
It is vital if you intend to supplement both B12 and folate that B12 is started a week before the folate.
At least 48 hours after first B12 injection GP should be prescribing folic acid for folate deficiency
When he finishes Folic acid supplement in 2-3 months
He can then start to self supplement a good quality daily vitamin B complex, one with folate in (not folic acid)
This can help keep all B vitamins in balance and will help improve B12 levels too
Difference between folate and folic acid
chriskresser.com/folate-vs-...
Many Hashimoto’s patients have MTHFR gene variation and can have trouble processing folic acid.
thyroidpharmacist.com/artic...
B vitamins best taken after breakfast
Thorne Basic B recommended vitamin B complex that contains folate, but they are large capsules. (You can tip powder out if can’t swallow capsule)
Thorne currently difficult to find at reasonable price, should be around £20
If you want to try a different brand in the meantime, one with virtually identical doses of the ingredients, and bioavailable too, then take a look at Vitablossom Liposomal B Complex. Amazon sometimes has it branded Vitablossom but it's also available there branded as Yipmai, it's the same supplement
amazon.co.uk/Yipmai-Liposom...
or available as Vitablossom brand here
hempoutlet.co.uk/vitablosso... &description=true
IMPORTANT......If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 7 days before ALL BLOOD TESTS , as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
In week before blood test, when he stops vitamin B complex, he might want to consider taking a separate methyl folate supplement and continue separate B12
With serum B12 result below 500, (Or active B12 below 70) recommended to be taking a B12 supplement as well as a B Complex (to balance all the B vitamins)
once serum B12 is over 500 (or Active B12 level has reached 70), may be able to stop the B12 and just carry on with the B Complex.
Low vitamin levels tend to lower TSH
As your son has severe vitamin D, folate and B12 deficiency in reality his TSH is likely significantly higher than 7
What were his thyroid results 2 years ago that endocrinologist incorrectly told him to stop levothyroxine?
He will need to SLOWLY increase levothyroxine upwards in 25mcg steps over coming months
But essential to get all four vitamins at optimal levels to help levothyroxine work well
His Tsh was 1.68 and his T4 was 21.5 and his T3 was 6 so good I think but he took him off 100mcg levo coz said he was subclinical
If he felt well at that time, then taking him off Levo when autoimmune thyroid disease had already been diagnosed was idiotic .Those result were good BECAUSE he was taking Levo.
This has made me so angry ...he has just started a new job and is now off sick 😫...can I just ask ...my son wants to lose weight because he has increase a lot and wants to do the Cambridge meal replacement diet. High protein low carb do uou think it would be OK for him
Absolutely not …. Shakes are full of soya
All thyroid patients need to avoid all soya
He needs good quality real food
Plenty of protein and good fats
Steak and salad
Salmon and broccoli and carrots
Etc etc
Limit beige carbs - potatoes, rice cakes etc
Highly likely to benefit from strictly gluten free diet
But get coeliac blood test done first
Weight will fall off once he’s on decent dose levothyroxine and all vitamins at optimal levels
Just back from doctors...shes refused to put him back on thyroxine or give him B12 supplements because she says they are all normal and she can't override the consultant and must wait for a TSH of 10.. basically sent him away with advice on alcohol use coz his liver enzymes are raised ..I'm so angry 😠 completely ignore me with my notes and dismissed all I said about treatment
make an appointment with different GP at same surgery NOW ….today
Vitamin D result is 7 (50-200)
Severely deficient
Folate result 1.1 (3-20)
Severely deficient
B12 Result 174 (200-910)
Severely deficient
Write letter to practice manager
With these results
Say GP has refused to treat
Print out this flow chart on starting levothyroxine
With TSH over 5, and high Thyroid antibodies and multiple vitamin deficiencies and symptoms he should be started back on levothyroxine IMMEDIATELY
Starting levothyroxine - flow chart
gps.northcentrallondonccg.n...
Roughly where in U.K. are you
Email Thyroid U.K. for list of thyroid specialist endocrinologists and doctors
tukadmin@thyroiduk.org
I couldn't get another appointment but have written an email to the practise manager and his usual doctor who is in tomorrow requesting an urgent review of his bloods and history ..insisting they start the correct treatment immediately. If I don't get the correct response will take further...
Has this GP prescribed folic acid supplements
With such low B12 he must not start any folic acid supplements or folate until 48 hours after first B12 injections or week after starting B12 daily supplements
Note that improving folate when B12 is very low is not a good idea. Taking folate before B12 is improved can lead to severe neurological problems.
en.wikipedia.org/wiki/Subac...
It is vital if you intend to supplement both B12 and folate that B12 is started a week before the folate.
suggest you ask advice on PAS Healthunlocked too
I don't often comment on other admin's good comments.
But this B12 issue cannot be overemphasised. B12 must be addressed before folate.
Lanvere I implore you to go to the Pernicious Anaemia Society forum (as linked above) and post there (as well as carrying on here).
He really needs to be tested for Intrinsic Factor antibodies.
as slowdragom says ... no , don't let him do 'dieting' .. do 'good quality food' with plenty of nutrients and protein in it , he needs it , and the weight will sort itself out once the thyroid is properly medicated again and over then next few months as his body and metabolism has chance to start working properly again .
I'm so angry for him too.
Get him put back on Levo NOW ....don't let him get fobbed off with "it might get better wait 3 months" etc .. Tell them his work is affected NOW and his job is at stake NOW, and they already have the diagnosis so they don't need to wait the usual 3 moths to confirm a raised TSH.. They already know it will only get worse due to the Hashimoto's diagnosis.
Make sure they start at 50mcg not 25mcg . be pushy , put the references we've given you under his and his GP's noses ~ and then make sure he get retested after 6 weeks on 50mcg and make sure they then increase the dose until he is well again .
Don't take no for an answer (and while you're at it , somebody needs to ask the GP why he was put/ kept on antidepressants instead of treating his existing already diagnosed condition , which is known to cause / worsen depression.)
Tell him to be optimistic , hopefully once back on levo he will begin to feel some improvements fairly soon, even within the first month , those improvements may not last for the the first 6 weeks .. improvement is likely to be a bit 'up and down' over the first 6 months or longer while the doses are increased .. it's a bit "2 steps forward , One step back" ... i was diagnosed with TSH 6.8 after being left untested for about 4 years while i got slowly worse while nobody realised hypothyroidism was the issue.
I started on 50mcg and i do remember saying to the 'i felt about 75% better for a couple of weeks , but now i don't" , but then as dose was increased to 100mcg i felt better for a few months until it need increasing again. to about 125 /150 ish .
once he is back on Levo , don't let them leave him with TSH 'just back in range' .. use this list of references to make sure GP's keeps increasing dose until he feels consistently well :
list of references recommending GP's keep TSH between about 0.5 -2/ 2.5 ish when on Levo : healthunlocked.com/thyroidu.... (-list-of-references-recommending-gps-keep-tsh-lower)
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
A Helpful Quote from another members GP ,on what to expect when starting treatment for hypothyroidism:
"The way my new GP described it was ..."You know how your body is continually breaking down and rebuilding itself? Well, the thyroid controls the rebuilding, so if it isn't working you carry on breaking down but don't rebuild properly. Your body now has a lot of catching up to do, which will take a minimum of 12 months, probably a lot longer...." or words to that effect. He also said it would be a saw tooth recovery (get better, go backwards a bit, get better, go backwards a bit) and he's been right so far."
NEVER agree to stopping levothyroxine or even reducing dose if Ft3 isn’t over range
His levels were GOOD because he was on replacement thyroid hormones
Now he’s extremely unwell and at risk of neurological damage through extremely deficient B12 and folate as direct result
I would put in official complaint regarding this endocrinologist …..once your son’s recovered
Lastly
He needs full iron panel test including ferritin
He also needs coeliac blood test
nice.org.uk/guidance/ng20/c...
1.1 Recognition of coeliac disease
1.1.1 Offer serological testing for coeliac disease to:
people with any of the following:
persistent unexplained abdominal or gastrointestinal symptoms
faltering growth
prolonged fatigue
unexpected weight loss
severe or persistent mouth ulcers
unexplained iron, vitamin B12 or folate deficiency
type 1 diabetes, at diagnosis
autoimmune thyroid disease, at diagnosis
irritable bowel syndrome (in adults)
first‑degree relatives of people with coeliac disease.
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances. Most common by far is gluten. Dairy is second most common.
According to Izabella Wentz the Thyroid Pharmacist approx 5% with Hashimoto's test positive for coeliac, but a further 80% find strictly gluten free diet helps or is essential due to gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and slowly lower TPO antibodies
While still eating high gluten diet ask GP for coeliac blood test first
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
pubmed.ncbi.nlm.nih.gov/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
Likely eventual dose levothyroxine based on weight
Typically will take 6-12 months to correct vitamin deficiencies and increase levothyroxine slowly up to full replacement dose
Gluten free- takes 6-12 months to heal gut
Thank you so much for your support on this ...its such a shame he started a new job in November and is now off sick but at least we now have something to work with ...I'm really angry the endo took him off levo ...he was doing OK and now it will take months to get him back on track
He will likely need months signed off work
All completely unnecessary
why on earth were bloods retested 6-8 weeks after stopping levothyroxine and again every 3 months
Extremely poor care
Because I don't think the gp has ever taken his thyroid seriously ...I can't find the copy of the endo letter but I'm sure it said something about retesting ...the doc remarked that they hadn't seen him in a while other than for his anti depressants and as he feels grotty all the time anyway he would not have thought to have asked to see her ...he lives alone in a flat so I'm not always aware of how he is and he seemed to be doing OK until his anxiety ent though the roof with the change in work
make sure B12 is started at least 48 hours BEFORE he starts folic acid supplement
Presumably GP has actually prescribed vitamin D at loading dose ?
300,000iu vitamin D in total over 6-8 weeks
Yes they have done that
Did she prescribe folic acid ?
If so …..do NOT start it
Insist on testing for Pernicious Anaemia and B12 injections FIRST
No and refused b12 supplementation said Active B12 is normal so doesn't need ...I written a letter of complaint
NHS doesn’t ever test active B12
What on earth is she on about
It was a cobalmin test with anything over 30 being normal but no upper limit his result said because active b12 was 68 not true deficiency so no action necessary...in my email I said as no upper limit result over 30 would always be normal so clearly 68 is not normal for him
So you are going to need to start him on separate B12 drops - or lozenges
Then after week taking B12 everyday add folic acid
B12 drops
healthunlocked.com/thyroidu...
natureprovides.com/products...
Or
B12 sublingual lozenges
amazon.co.uk/Jarrow-Methylc...
cytoplan.co.uk/shop-by-prod...
B12 range in U.K. is too wide
Interesting that in this research B12 below 400 is considered inadequate
Has GP organised blood test for coeliac disease
If not get that booked up now
And ultrasound scan of thyroid too