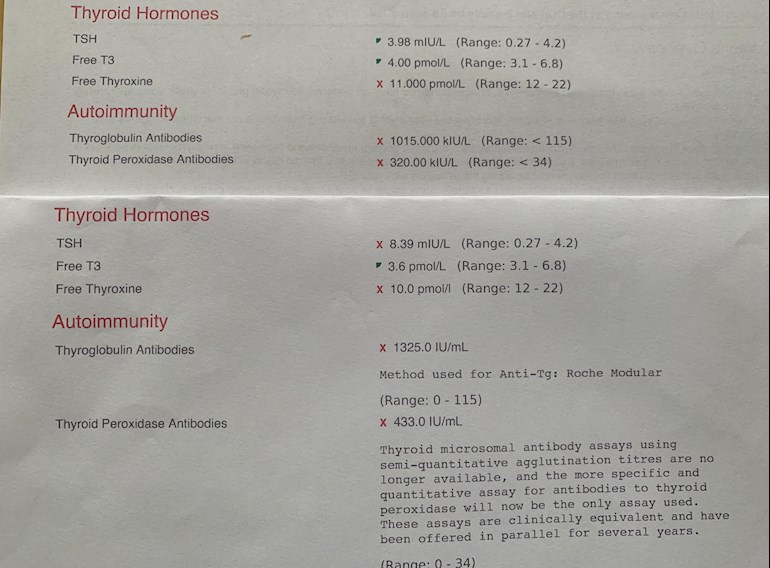
Hello all I am hypo after 2 year fight GP relented and gave me levo 50mcg, perimenaupause with GI issues high bp and now high cholesterol (GP sent me email to say it was high and website link for government site, no conversation…). Feeling continuously unwell, mood lethargy energy etc I paid for 2 x bloods 3 months apart, fasting in the morning no levo since 24 hr -pic attached. Any thoughts or insight most gratefully received feel unsupported by GP and at a loss. Have done some research and am non dairy, gluten and watch carbs have reflux and on omeprazole, thanks for reading
Puzzled hashimoto or not unsupportive GP - Thyroid UK
Puzzled hashimoto or not unsupportive GP
High cholesterol is linked to hypothyroidism *. NHS know this.
Properly treating the hypothyroidism should reduce the cholesterol.
Which of those tests is the latest one ?
mind you whichever it is , you re still clearly undermedicated and your GP should be to increasing the dose of Levothyroxine by 25mcg immediately
(Because the free T4 (thyroxine ) is under range on both, and 'optimally' treated patients on Levothyroxine should have TSH under 2 * )
We have several references for this * if you need them to show GP
Thank you for reply the bottom one is latest, will read up thank you any supporting evidence for levo increase gratefully received my GP is not supportive
OK, will look them up now , but if the latest one is 8.39 . you should get an increase with no bother.
even TSH of 3.98 is still too high for someone on Levo (unless you felt well )
So GP should increase levo by 25mcg as a result of either of these tests .
References for keeping TSH lower in ALL patients:
This one ..... from page 13 in the liothyronine (T3) guidance... sps.nhs.uk/wp-content/uploa...
" NHS consultant endocrinologists may start a trial of combination levothyroxine and liothyronine in circumstances where all other treatment options have been exhausted.
1. Where symptoms of hypothyroidism persist despite optimal dosage with levothyroxine.
(TSH 0.4-1.5mU/L)
2. Where alternative causes of symptoms have been excluded, see box 1 below"
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
This one ..... from PULSE magazine for GP's... The article is available from ThyroidUK
If you want a copy of the article then email tukadmin@thyroidUK.org
and ask for a copy of the Dr Toft article in Pulse magazine. The quote is in answer to question 6.
Dr Toft, past president of the British Thyroid Association and leading endocrinologist, states in Pulse Magazine:
"The appropriate dose of levothyroxine is that which restores euthyroidism and serum TSH to the lower part of the reference range - 0.2-0.5mU/l.
In this case, free thyroxine is likely to be in the upper part of its reference range or even slightly elevated – 18-22pmol/l.
Most patients will feel well in that circumstance.
But some need a higher dose of levothyroxine to suppress serum TSH and then the serum-free T4 concentration will be elevated at around 24-28pmol/l.
This 'exogenous subclinical hyperthyroidism' is not dangerous as long as serum T3 is unequivocally normal – that is, serum total around T3 1.7nmol/l (reference range 1.0-2.2nmol/l)."
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
This Graph showing TSH in healthy population ..... originalText (show's most are around 1 , 4 is extremely rare in healthy people )
and a post on here discussing it: healthunlocked.com/thyroidu...
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
plus This one ........ found in GPonline.com 15th April 2010.
gponline.com/endocrinology-...
"Replacement therapy with levothyroxine should be initiated in all patients to achieve a TSH level of 0.5-2.0pmol/L." Written for GP's by "Dr Iqbal is a specialist registrar in endocrinology and Dr Krishnan is a specialist registrar in cardiology, Liverpool".
* NOTE this one also clearly states that raised cholesterol is caused by hypothyroidism *
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Oh and This one .... gpnotebook.com/en-gb/simple...
"The goal of treatment is to make the patient feel better and this tends to correspond with a TSH in the lower half of the reference range (0.4–2.5 mU/l).
If a patient feels perfectly well with TSH between 2.5 and 5 mU/l there is no need to adjust the dosage" .
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
and another one .....
ncbi.nlm.nih.gov/pmc/articl...
"Given the complexity of pathways that govern TH action at tissue and cellular levels, it is not surprising that some patients receiving exogenous thyroid hormone replacement therapy report on-going symptoms despite optimal thyroid function tests
(e.g. normal T4 and T3 with TSH <2 mU/L in primary hypothyroidism).
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
frontiersin.org/articles/10...
A Renewed Focus on the Association Between Thyroid Hormones and Lipid Metabolism
Leonidas H. Duntas1* and Gabriela Brenta2 Treatment With L-T4: Why, Who, and How~
....therefore, TSH values can be considered a good predictor of cardiovascular disease, notably when its levels are above 10 mIU/L (75). In particular, a TSH above 2.5 mIU/L in women of childbearing age may induce oxidative damage to membrane lipids and unfavorably alter the lipid profile, suggesting that TSH levels in this population should preferably be maintained below 2.5 mIU/L (76) ".
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
just adding this so i can find it again later :
MHRA Safety update re. switching brands of Levo gov.uk/drug-safety-update/l... "If a patient reports persistent symptoms when switching between different levothyroxine tablet formulations, consider consistently prescribing a specific product known to be well tolerated by the patient. If symptoms or poor control of thyroid function persist (despite adhering to a specific product), consider prescribing levothyroxine in an oral solution formulation."
Presumably the top results are after being on 50mcg levothyroxine
How long on this dose
Bloods should be retested 6-8 weeks after each dose change or brand change in levothyroxine
50mcg is only a STARTER dose
The aim of levothyroxine is to increase the dose slowly upwards in 25mcg steps until TSH is ALWAYS under 2
Most important results are always Ft4 and Ft3
When adequately treated Ft4 will be 60-70% through range and Ft3 at least 60% through range
See/contact GP for next increase in levothyroxine up to 75mcg per day
Essential to test vitamin D, folate, ferritin and B12 too
Have you had these tested, highly likely low
Thank you for reply, 4 years GP adamant that dose is correct and will not prescribe higher despite, symptoms continuing. no repeat bloods ever after brand change (did not know this was a thing) standard 6 month bloods requested only. I have constant reflux which is helped by omeprazole only take when it’s very bad though. Pic attached recent bloods
Hi I don't see acid reflux mentioned that often with hypothyroidism but it was definitely something that thyroid treatment improved for me. I was on daily omeprazole, also laxatives and suppositories which are no longer needed. I am still struggling with other issues but I found GI issues the first thing that thyroid treatment eliminated.
How long have you been on omeprazole?
Most hypothyroid patients have LOW stomach acid
Any PPI like omeprazole is to treat high stomach acid
Low stomach acid can be a common hypothyroid issue
Thousands of posts on here about low stomach acid
healthunlocked.com/search/p...
Web links re low stomach acid and reflux and hypothyroidism
nutritionjersey.com/high-or...
articles.mercola.com/sites/...
thyroidpharmacist.com/artic...
stopthethyroidmadness.com/s...
healthygut.com/articles/3-t...
naturalendocrinesolutions.c...
meraki-nutrition.co.uk/indi...
huffingtonpost.co.uk/laura-...
lispine.com/blog/10-telling...
Protect your teeth if using ACV with mother
healthunlocked.com/thyroidu...
Ppi
Omeprazole will tend lower vitamin levels even further
gov.uk/drug-safety-update/p...
webmd.com/heartburn-gerd/ne...
pharmacytimes.com/publicati...
PPI and increased risk T2 diabetes
gut.bmj.com/content/early/2...
Iron Deficiency and PPI
medpagetoday.com/resource-c...
futurity.org/anemia-proton-...
onlinelibrary.wiley.com/doi...
sciencedirect.com/science/a...
You must not simply stop PPI
Getting levothyroxine dose increase is first step
Being hypothyroid causes low stomach acid, increasing levothyroxine dose should help improve gut function
Testing vitamins absolutely essential
Come back with new post once you get vitamin D, folate, ferritin and B12 test results
Private tests are available as NHS currently rarely tests Ft3 or all relevant vitamins
List of private testing options
thyroiduk.org/getting-a-dia...
Medichecks Thyroid plus antibodies and vitamins
medichecks.com/products/adv...
Blue Horizon Thyroid Premium Gold includes antibodies, cortisol and vitamins by DIY fingerprick test
bluehorizonbloodtests.co.uk...
NHS easy postal kit vitamin D test £29 via
HelloI’m sorry you are feeling so bad. Meno on top of thyroid issues is extremely tough- I’m suffering along side you atm.
Your results indicate Hashimoto’s as both antibodies over range and you are under medicated for thyroid. But likely they’ll only increase after 6-8 weeks by 25mcg. And you’ll have to ask for it in my experience with NHS GP blood tests will need repeating first. Problem is, they’ll only check TSH which is why so many of us end up spending money we don’t have on private thyroid sympathetic GPS and private bloods, as you’ve discovered. I’m sure The more experienced and knowledgable will be along shortly with more suggestions.
Your journey is a mirror of mine and I’m in full sympathy with you x
Thank you wishing you well I will keep fighting
High cholesterol is linked to being under medicated for thyroid
Your GP should be aware of this (rarely seem to be)
nhs.uk/conditions/statins/c...
If you have an underactive thyroid (hypothyroidism), treatment may be delayed until this problem is treated. This is because having an underactive thyroid can lead to an increased cholesterol level, and treating hypothyroidism may cause your cholesterol level to decrease, without the need for statins. Statins are also more likely to cause muscle damage in people with an underactive thyroid.
Getting dose levothyroxine increased will reduce cholesterol
Guidelines on eventual dose levothyroxine likely to need is approx 1.6mcg per kilo of your weight
Dose has to usually be increased slowly upwards in 25mcg steps, retesting 6-8 weeks after each increase
guidelines on dose levothyroxine by weight
Even if we frequently don’t start on full replacement dose, most people need to increase levothyroxine dose slowly upwards in 25mcg steps (retesting 6-8 weeks after each increase) until eventually on, or near full replacement dose
NICE guidelines on full replacement dose
nice.org.uk/guidance/ng145/...
1.3.6
Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
Also here
cks.nice.org.uk/topics/hypo...
gp-update.co.uk/Latest-Upda...
Traditionally we have tended to start patients on a low dose of levothyroxine and titrate it up over a period of months. RCT evidence suggests that for the majority of patients this is not necessary and may waste resources.
For patients aged >60y or with ischaemic heart disease, start levothyroxine at 25–50μg daily and titrate up every 3 to 6 weeks as tolerated.
For ALL other patients start at full replacement dose. For most this will equate to 1.6 μg/kg/day (approximately 100μg for a 60kg woman and 125μg for a 75kg man).
If you are starting treatment for subclinical hypothyroidism, this article advises starting at a dose close to the full treatment dose on the basis that it is difficult to assess symptom response unless a therapeutic dose has been trialled.
BMJ also clear on dose required
Notdepressed
Definitely Hashi's.
Some information about Hashi's:
stopthethyroidmadness.com/h...
stopthethyroidmadness.com/h...
hypothyroidmom.com/hashimot...
thyroiduk.org.uk/tuk/about_...
Supplementing with selenium l-selenomethionine 200mcg daily is said to help reduce the antibodies, as can keeping TSH suppressed.
How long have you been on 50mcg Levo?
Retesting with GP should be 6 weeks after starting Levo, increase by 25mcg, retest 6-8 weeks later, repeat until levels are where you need them to be for you to feel well.
The aim of a Hypo patient on Levo only, generally, is for TSh to be 1 or below with FT4 and FT3 in the upper part of their reference ranges, if that is where you feel well.
If GP is reluctant to retest/increase then use the NICE guidelines which he may be ignorant of:
nice.org.uk/guidance/ng145/...
1.4 Follow-up and monitoring of primary hypothyroidism
Tests for follow-up and monitoring of primary hypothyroidism
1.4.1 Aim to maintain TSH levels within the reference range when treating primary hypothyroidism with levothyroxine. If symptoms persist, consider adjusting the dose of levothyroxine further to achieve optimal wellbeing, but avoid using doses that cause TSH suppression or thyrotoxicosis.
1.4.2 Be aware that the TSH level can take up to 6 months to return to the reference range for people who had a very high TSH level before starting treatment with levothyroxine or a prolonged period of untreated hypothyroidism. Take this into account when adjusting the dose of levothyroxine.
Adults
1.4.3 For adults who are taking levothyroxine for primary hypothyroidism, consider measuring TSH every 3 months until the level has stabilised (2 similar measurements within the reference range 3 months apart), and then once a year.
1.4.4 Consider measuring FT4 as well as TSH for adults who continue to have symptoms of hypothyroidism after starting levothyroxine.
Hashi's isn't treated, it's the resulting hypothyroidism that is.
Hashi's can cause gut/absorption issues so it's important to test key nutrients as these are often low or deficient:
Vit D
B12
Folate
Ferritin
High cholesterol is one of the signs/symptom of hypothyroidism, avoid statins if they are offered, hypothyroidism has to be treated before considering statins:
nhs.uk/conditions/statins/c...
If you have an underactive thyroid (hypothyroidism), treatment may be delayed until this problem is treated. This is because having an underactive thyroid can lead to an increased cholesterol level, and treating hypothyroidism may cause your cholesterol level to decrease, without the need for statins. Statins are also more likely to cause muscle damage in people with an underactive thyroid.
High blood pressure is another of the signs/symptoms of hypothyroidism so that may improve.
Which brand of levothyroxine are you currently taking
Many people find different brands are not interchangeable
Best to not change brand at dose increase
Many patients do NOT get on well with Teva brand of Levothyroxine.
Teva contains mannitol as a filler, which seems to be possible cause of problems. Teva is the only brand that makes 75mcg tablet. So if avoiding Teva for 75mcg dose ask for 25mcg to add to 50mcg or just extra 50mcg tablets to cut in half
But for some people (usually if lactose intolerant, Teva is by far the best option)
Teva, or Aristo (100mcg only) are the only lactose free tablets
Most easily available (and often most easily tolerated) are Mercury Pharma or Accord
Mercury Pharma make 25mcg, 50mcg and 100mcg tablets
Accord only make 50mcg and 100mcg tablets
Accord is also boxed as Almus via Boots, and Northstar 50mcg and 100mcg via Lloyds ....but Accord doesn’t make 25mcg tablets
beware 25mcg Northstar is Teva
List of different brands available in U.K.
thyroiduk.org/if-you-are-hy...
Posts that mention Teva
healthunlocked.com/search/p...
Teva poll
healthunlocked.com/thyroidu...
Once you find a brand that suits you, best to make sure to only get that one at each prescription.
Watch out for brand change when dose is increased or at repeat prescription.
New guidelines for GP if you find it difficult/impossible to change brands
gov.uk/drug-safety-update/l...
If a patient reports persistent symptoms when switching between different levothyroxine tablet formulations, consider consistently prescribing a specific product known to be well tolerated by the patient. If symptoms or poor control of thyroid function persist (despite adhering to a specific product), consider prescribing levothyroxine in an oral solution formulation.
academic.oup.com/jcem/artic...
Physicians should: 1) alert patients that preparations may be switched at the pharmacy; 2) encourage patients to ask to remain on the same preparation at every pharmacy refill; and 3) make sure patients understand the need to have their TSH retested and the potential for dosing readjusted every time their LT4 preparation is switched (18).
Levothyroxine is an extremely fussy hormone and should always be taken on an empty stomach and then nothing apart from water for at least an hour after
Many people take Levothyroxine soon after waking, but it may be more convenient and perhaps more effective taken at bedtime
verywellhealth.com/best-tim...
No other medication or supplements at same as Levothyroxine, leave at least 2 hour gap.
Some like iron, calcium, magnesium, HRT, omeprazole or vitamin D should be four hours away
(Time gap doesn't apply to Vitamin D mouth spray)
If you normally take levothyroxine at bedtime/in night ...adjust timings as follows prior to blood test
If testing Monday morning, delay Saturday evening dose levothyroxine until Sunday morning. Delay Sunday evening dose levothyroxine until after blood test on Monday morning. Take Monday evening dose levothyroxine as per normal
You are clearly hypothyroid. Ask your doctor about link with hypothyroidism and high cholesterol. Mine still didn't care despite acknowledging I had a point, but you could use that as a basis for an increase.
Failing that try and change doctors or sorry, go private
The next step from here from your doctors point of view is BP tablets and Statins, both of which make thyroid hormone conversion harder. Many years ago when I was fairly ignorant I saw a very good private functional doctor (former GP with hypothyroidism) His words to me as the consultation finished were: "No matter what, don't let any doctor put you on statins, eat as much fat as you like, yes eat butter! I recommend it, it will do you no harm, our cells need fat, and you need all the energy you can get, but don't let them tell you your high cholesterol is due to your diet! Your high cholestrol is currently saving you from complete collapse."
I left thinking (I truly was ignorant) that he was overly zealous.
But he was dead right and I am very grateful for his words.
Dear Alanna012,
Your post (the comments of the private functional doctor, a former GP with hypothyroidism, especially his final sentence) was worth its weight in gold to me. Thanks so much for sharing.
To you and all the others on Thyroid UK, valued Administrators included, my heartfelt wishes for far better health,
Chrysalis56
Ps The cholesterol is often raised with Hyoo- mine as mine has been for a long time and I’m apparently at optimum dose.
Blood pressure swings up and down with Hashi flairs (I’ve had 2 significant bouts so debilitating unable to work for a period of time once 2 years ago & currently battling the tail end of flair 2) but usually when reasonably controlled T the lower end.
Re flairs: looking back, I see the pattern. Was fine last winter (a miracle) Sick the one before, ok one before that and sick the year before. I thought that was flu bug as not diagnosed then but I now know it was thyroid flair. Winter notoriously hard to control symptoms for some as body working harder to keep you warm. Some docs automatically increase dosage ready for winter months, I believe.
It’s a tricky condition and thank goodness for the help on here from the experienced. It’s got me through some difficult times
X
Thank you I’ve not been diagnosed hashimoto I suspect it will read up about thyroid flares are there any good sites of information, hoping you stay well
"I’ve not been diagnosed hashimoto" If the GP has ever done a TPOab (antibody) test and it was over range then you have already been diagnosed with it ....
.. they just didn't mention it , they often don't bother because it makes no difference to treatment of hypothyroidism.. or if they did mention it they didn't use the term 'hashimotos ' most GP's would only call it "Autoimmune Hypothyroidism".. but because this is the most common reason for becoming hypothyoid ., they often don't mention it at all .. and just write "hypothyroidism"
Important ...if TSH is now 8 you need to contact GP and let them know this... there is no question (even for the most unhelpful GP in the world) that a TSH of 8 is not OK once they are treating you with Levo .. they are clearly instructed to adjust Levo dose to get TSH into range
Seaside Susie’s links are really useful for explaining Hashis and there’s lots in line re Hashimoto’s Thyroiditis but likely you’ll need a thyroid scan to validate this recently after my current flair and ensuing illness. I paid for a private one and it was confirmed this way, but had really high antibodies a couple of years ago when first diagnosed by private GP. Both antibodies over range. Tbh NHS GPS are mainly not remotely interested in testing for antibodies so you’d have to go private or ask for referral to Endo.
I had one Endo who completely dismissed my high antibodies and blamed everything on my menopause and wanted to take me off Levo!! Needless to say, I didn’t go back. And that was a private referral. I then stuck with my private GP who is all over thyroid and treating the symptoms not the numbers.
To be fair to GPS they are general practice and won’t know everything about a specific condition- that’s the place for a specialist. However, it’s just about finding a doctor who’s willing to listen. Sadly, we get dismissed as menopausal or having depression/ anxiety or health anxiety rather than listening.
I’m all for trusting and listening to your body. I did and bingo- T4 over range and low T3 and an abnormal thyroid scan. All paid for privately but at least it gave me confirmation I wasn’t going mad or suffering from a panic disorder.
Keep faith in yourself. You know your own body.
It’s a battle so keep fighting 🤗
Thank you I will be making an appointment armed with all this information from replies have felt at a total loss recently but everyone’s help has really boosted me thank you
Ft4 is BELOW RANGE
When adequately treated Ft4 will be minimum 60% through range
Likely to need several further increases over coming months
