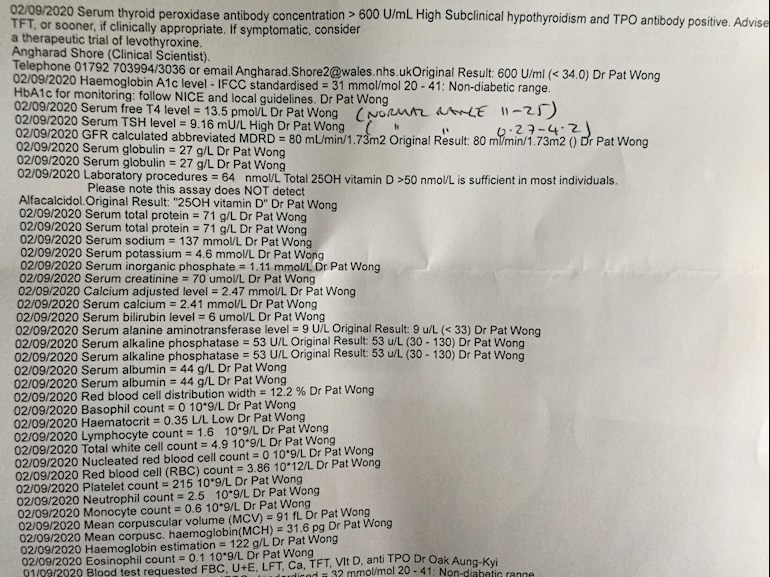
Would someone be able to help me interpret these results please? I have been suffering with fatigue, weight gain, depression and lack of motivation and believe I may have a thyroid issue. Doctor doesn’t seem concerned and has advised me to retest in 6 months. Many thanks.
Thyroid Problem?! Help please! : Would someone be... - Thyroid UK
Thyroid Problem?! Help please!
Welshbetty77
Doctor doesn’t seem concerned and has advised me to retest in 6 months.
Well, your doctor should be concerned and would do well to read the top bit of this print out as it's quite plain that you have autoimmune thyroid disease (known to patients as Hashimoto's).
Serum thyroid peroxidase antibodies >600
High subclinical hypothyroidism and TPO antibody positive
If symptomatic consider a therapeutic trial of levothyroxine
Your TSH is marked as high, it's way over range and very close to the magic 10 that is used to diagnose Primary Hypothyroidism.
You have symptoms which, if you have mentioned them to your GP, should know that they can be symptoms of hypothyroidism and the print out says to consider a trial of levothyroxine if symptomatic.
With an over range, but under 10, TSH with positive antibodies you should be prescribed Levo according to NICE guidelines:
nice.org.uk/guidance/ng145/...
Treating subclinical hypothyroidism
1.5.2 When discussing whether or not to start treatment for subclinical hypothyroidism, take into account features that might suggest underlying thyroid disease, such as symptoms of hypothyroidism, previous radioactive iodine treatment or thyroid surgery, or raised levels of thyroid autoantibodies.
1.5.4 Consider a 6-month trial of levothyroxine for adults under 65 with subclinical hypothyroidism who have:
a TSH above the reference range but lower than 10 mlU/litre on 2 separate occasions 3 months apart, and
symptoms of hypothyroidism.
If symptoms do not improve after starting levothyroxine, re-measure TSH and if the level remains raised, adjust the dose. If symptoms persist when serum TSH is within the reference range, consider stopping levothyroxine and follow the recommendations on monitoring untreated subclinical hypothyroidism and monitoring after stopping treatment.
and Dr Toft, past president of the British Thyroid Association and leading endocrinologist, states in Pulse Magazine (the magazine for doctors):
Question 2:
I often see patients who have an elevated TSH but normal T4. How should I be managing them?
Answer:
The combination of a normal serum T4 and raised serum TSH is known as subclinical hypothyroidism. If measured, serum T3 will also be normal. Repeat thyroid function tests in two or three months in case the abormality represents a resolving thyroiditisis.
But if it persists then antibodies to thyroid peroxidase should be measured. If these are positive - indicative of underlying autoimmune disease - the patient should be considered to have the mildest form of hypothyroidism.
In the absence of symptoms some would simply recommend annual thyroid function tests until serum TSH is over 10mU/l or symptoms such as tiredness and weight gain develop. But a more pragmatic approach is to recognise that the thyroid failure is likely to be come worse and try to nip things in the bud rather than risk loss to follow up.
Treatment should be started with levothyroxine in a dose sufficient to restore serum TSH to the lower part of it's reference range. Levothyroxine in a dose of 75-100mcg daily will usually be enough.
If there are no thyroid peroxidase antibodies, levothyroxine should not be started unless serum TSH is consistently greater than 10mU/l. A serum TSh of less than 10mU/l in the absence of antithyroid peroxidase antibodies may simply be that patient's normal TSH concentration.
Show this evidence to your GP and ask for a trial of Levothyroxine with a starting dose of no less than 50mcg unless you are over 60 or have a heart condition then you may be restricted to a starting dose of 25mcg.
Vit D: 64nmol/L
The Vit D Council recommends a level of 125nmol/L and the Vit D Society recommends a level of 100-150nmol/L.
Your GP will not prescribe at your level so if you want to improve it you will need to buy your own D3 supplement.
To reach the recommended level from your current level, based on the Vit D Council's suggestions you could supplement with 3,500-4,000iu D3 daily.
Retest after 3 months which you will have to do privately as most GPs wont repeat Vit D test.
Once you've reached the recommended level then you'll need a maintenance dose to keep it there, which may be 2000iu daily, maybe more or less, maybe less in summer than winter, it's trial and error so it's recommended to retest once or twice a year to keep within the recommended range. You can do this with a private fingerprick blood spot test with an NHS lab which offers this test to the general public:
Doctors don't know, because they're not taught much about nutrients, but there are important cofactors needed when taking D3 as recommended by the Vit D Council.
D3 aids absorption of calcium from food and Vit K2-MK7 directs the calcium to bones and teeth where it is needed and away from arteries and soft tissues where it can be deposited and cause problems such as hardening of the arteries, kidney stones, etc.
D3 and K2 are fat soluble so should be taken with the fattiest meal of the day, D3 four hours away from thyroid meds if taking D3 as tablets/capsules/softgels, no necessity if using an oral spray.
Magnesium helps D3 to work. We need Magnesium so that the body utilises D3, it's required to convert Vit D into it's active form. So it's important we ensure we take magnesium when supplementing with D3.
Magnesium comes in different forms, check to see which would suit you best and as it's calming it's best taken in the evening, four hours away from thyroid meds if taking magnesium as tablets/capsules, no necessity if using topical forms of magnesium.
naturalnews.com/046401_magn...
drjockers.com/best-magnesiu...
Thank you so much for this; just as I thought really but being totally new to this wanted to check as I could have been misreading...although, as you say the top of the printout couldn’t be clearer really! Would people ask to be referred to a consultant endocrinologist in this case or ask the doctor directly for the medication? Thanks once again.
Betty
Are you in Wales? The reason I ask is because I am and my health board is BCUHB. If that's your health board then I would strongly recommend you don't see an endo at either of the main hospitals, but that's just my experience (maybe some people have had a good outcome).
Personally, I think your results speak for themselves and it's as clear as day that you need treatment and your GP can sort this out - start you on Levo, retest after 6 weeks, increase dose of Levo, retest 6-8 weeks later, repeat until your levels are where they need to be for you to feel well.
The Hashi's slightly complicates things, I'm just going to log o to my computer (on tablet at the moment) where I have information stored so that I can pass it on to you.
Thanks so much once again: I am in Wales and my health board is Swansea Bay UHB. I'm one of these people who has hardly ever been treated for anything; rarely go to the doctors and had to google who my health board was as I didn't even know that! So your knowledge really is so helpful and appreciated. I've been feeling this way for a number of years now, but with young children, and some huge changes, I've put it all down to just life! I've also developed something called PMLE which is sun allergy and I'm pretty convinced this and the thyroid issues are linked. I've also dabbled in supplementing and taking various vitamins to boost my low mood and lack of motivation...probably to no avail as I've no idea what I've really been doing! I had my vitamin B12 test included last year which came back as 405 ng/L and the Dr said they wouldn't test this time as that is an adequate store for two years. Thank you again for your time and knowledge. X
Betty
Although within range and your GP would be happy enough with your B12 result, it was low. Neurological problems can occur when it's below 550ng/L.
We shouldn't take certain vitamins without first testing as some get stored in our body and ca lead to toxicity, so we always advise testing first. If your GP won't do them then we can do them with one of our recommended private labs and they can often be done with a fingerprick test at home.
Betty
OK, back again 
Hashi's is where the immune system attacks the thyroid and gradually destroys it. Hashi's is the most common cause of hypothyroidism.
Fluctuations in symptoms and test results tend to happen when Hashi's is present.
Most doctors dismiss antibodies as being of no importance and know little or nothing about Hashi's and how it affects the patient, test results and symptoms. You need to read, learn, understand and help yourself where Hashi's is concerned.
Some members have found that adopting a strict gluten free diet can help, although there is no guarantee.
Gluten contains gliadin (a protein) which is thought to trigger autoimmune attacks so eliminating gluten can possibly help reduce these attacks.
You don't need to be gluten sensitive or have Coeliac disease for a gluten free diet to help.
Gluten/thyroid connection: chriskresser.com/the-gluten...
stopthethyroidmadness.com/h...
stopthethyroidmadness.com/h...
hypothyroidmom.com/hashimot...
thyroiduk.org.uk/tuk/about_...
Supplementing with selenium l-selenomethionine 200mcg daily is said to help reduce the antibodies, as can keeping TSH suppressed (of course, you have to be on Levo to bring your TSH down).
Hashi's and gut absorption problems tend to go hand in hand and can very often result in low nutrient levels or deficiencies. It's essential to test Vit D, B12, Folate and Ferritin and address any problems. We already know about your Vit D so if you can get the others tested you are welcome to post these results, including reference ranges (plus units of measurement forB12) for comment and suggestions for supplementing where necessary.
**
The aim of a treated hypo patient on Levo, generally, is for TSH to be 1 or below with FT4 and FT3 in the upper part of their reference ranges if that is where you feel well.
Dr Wrong 🤣