Hi I’ve been diagnose with hypothyroidism. I’m on 50 levothyroxine and had a blood test 8 weeks later. Thyroid test has now come back normal’ but they also did an antibody test which has come back abnormal. Does this mean the dose of my meds need changing? Does this mean I have Hashimotos? Sorry I’m so clueless and find it difficult to understand/interperate results. I can’t get a drs app until end of next week. I’d appreciate any insight.
Hashimoto?: Hi I’ve been diagnose with... - Thyroid UK
Hashimoto?
Antibodies would indicate Hashimoto’s. This does not automatically mean you need a dose increase. That will depend on your thyroid Test results (TSH, T4 and T3). What does the doctor mean by ‘normal’ for your TSH? And how do you feel? If you ask for a print out of your results and post them on this forum, others may be able to advise, especially if you are still having symptoms.
Please add actual results and ranges on TSH and Ft4 (and Ft3 if it was tested)
High TPO antibodies confirms cause of your hypothyroidism is autoimmune thyroid disease also called Hashimoto’s
EXTREMELY important to test vitamin D, folate, ferritin and B12
Low vitamin levels are extremely common with Hashimoto’s
Ask GP to test vitamin levels
Recommended on here that all thyroid blood tests should ideally be done as early as possible in morning and before eating or drinking anything other than water .
Last dose of Levothyroxine 24 hours prior to blood test. (taking delayed dose immediately after blood draw).
This gives highest TSH, lowest FT4 and most consistent results. (Patient to patient tip, best not mentioned to GP or phlebotomist)
Is this how you do your tests?
Private tests are available as NHS currently rarely tests Ft3 or thyroid antibodies or all relevant vitamins
List of private testing options
thyroiduk.org/getting-a-dia...
50mcg levothyroxine is only a starter dose
Typically dose is increased slowly upwards in 25mcg steps, retested 6-8 weeks after each dose increase until on full replacement dose
NICE guidelines on full replacement dose
nice.org.uk/guidance/ng145/...
1.3.6
Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
gp-update.co.uk/Latest-Upda...
Traditionally we have tended to start patients on a low dose of levothyroxine and titrate it up over a period of months.
RCT evidence suggests that for the majority of patients this is not necessary and may waste resources.
For patients aged >60y or with ischaemic heart disease, start levothyroxine at 25–50μg daily and titrate up every 3 to 6 weeks as tolerated.
For ALL other patients start at full replacement dose. For most this will equate to 1.6 μg/kg/day (approximately 100μg for a 60kg woman and 125μg for a 75kg man).
If you are starting treatment for subclinical hypothyroidism, this article advises starting at a dose close to the full treatment dose on the basis that it is difficult to assess symptom response unless a therapeutic dose has been trialled.
A small Dutch double-blind cross-over study (ArchIntMed 2010;170:1996) demonstrated that night time rather than morning dosing improved TSH suppression and free T4 measurements, but made no difference to subjective wellbeing. It is reasonable to take levothyroxine at night rather than in the morning, especially for individuals who do not eat late at night.
BMJ also clear on dose required
bestpractice.bmj.com/topics...
Add any vitamin results and ranges if you have them
Or come back with new post once you get results
JuneSerum free T4: 6.9pmol/L
(7.86–14.41)
TSH: 9.56 mu/L
(0.35-5.5)
Ferritin: 29.5ug/L
(22–322)
Aug
Free T4: 8.1
TSH: 3.08
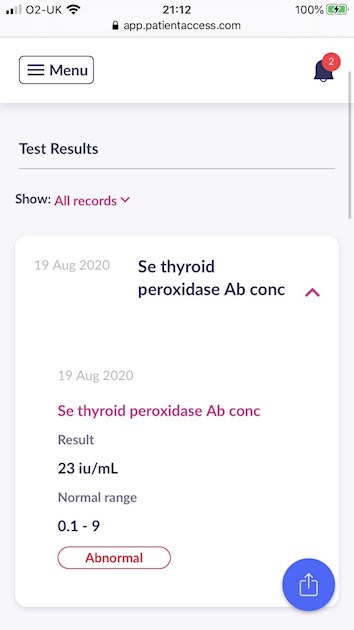
Antibody in pic above
So you need 25mcg dose increase in levothyroxine and bloods retested in 6-8 weeks
Aim is to increase the dose until Ft4 is in top third. Of range and Ft3 at least 50% of range
Essential to test vitamin D, folate, ferritin and B12
According to Izabella Wentz the Thyroid Pharmacist approx 5% with Hashimoto's are coeliac, but over 80% find gluten free diet helps, sometimes significantly. Either due to direct gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and slowly lower TPO antibodies
While still eating high gluten diet ask GP for coeliac blood test first or buy test online for under £20, just to rule it out first
healthcheckshop.co.uk/store...?
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
restartmed.com/hashimotos-g...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
ncbi.nlm.nih.gov/pubmed/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
ncbi.nlm.nih.gov/pubmed/300...
The obtained results suggest that the gluten-free diet may bring clinical benefits to women with autoimmune thyroid disease
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
Official NHS guidelines saying TSH should be between 0.2 and 2.0 when on Levothyroxine
(Many of us need TSH nearer 0.2 than 2.0 to feel well)
See box
Thyroxine replacement in primary hypothyroidism
Many people find Levothyroxine brands are not interchangeable.
Once you find a brand that suits you, best to make sure to only get that one at each prescription.
Watch out for brand change when dose is increased or at repeat prescription.
Many patients do NOT get on well with Teva brand of Levothyroxine. Teva contains mannitol as a filler, which seems to be possible cause of problems. Teva is the only brand that makes 75mcg tablet. So if avoiding Teva for 75mcg dose ask for 25mcg to add to 50mcg or just extra 50mcg tablets to cut in half
Teva and Aristo are the only lactose free tablets
healthunlocked.com/thyroidu...
Teva poll
healthunlocked.com/thyroidu...
academic.oup.com/jcem/artic...
Physicians should: 1) alert patients that preparations may be switched at the pharmacy; 2) encourage patients to ask to remain on the same preparation at every pharmacy refill; and 3) make sure patients understand the need to have their TSH retested and the potential for dosing readjusted every time their LT4 preparation is switched (18).
Levothyroxine is an extremely fussy hormone and should always be taken on an empty stomach and then nothing apart from water for at least an hour after
Many people take Levothyroxine soon after waking, but it may be more convenient and perhaps more effective taken at bedtime
verywellhealth.com/best-tim...
No other medication or supplements at same as Levothyroxine, leave at least 2 hour gap. Some like iron, calcium, magnesium, HRT, omeprazole or vitamin D should be four hours away
(Time gap doesn't apply to Vitamin D mouth spray)
I am equally clueless ! I’m about to have my first 8 week blood test.
What’s the antibody test for?