Well that was quick, for the thyroid tests, my vitamin levels were a separate sample, results not through yet.
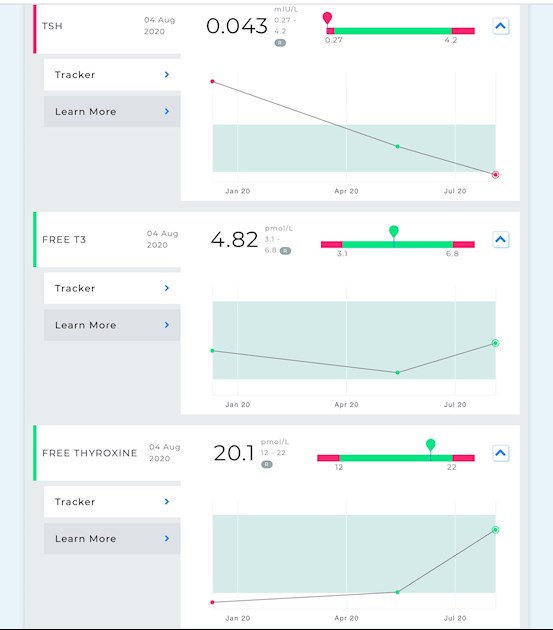
December 2019, before treatment.
Feb 2020’ started on 50mcg levo, after doc tests where TSH was similar to the medichecks result.
May 2020, results after 8 weeks of 50mcg.
Doc result, TSH only, 4.3 (0.27-4.2), dose increase to 100mcg.
August 2020, results below and the trend line from the previous medichecks tests.
When doc increased the dose he said to check again (with his blood check) in 3 months or if I felt well in 6 months. I’d told him about the May medichecks test and he probably figured (rightly) that I’d do another test myself and get back to him if not all right.
I’m feeling mostly alright, my hair is shedding but that may be because it’s longer than normal so I’m noticing it more. The air hunger is better, I’m not ‘yawning’ as much as I was. Running is ok until I find a hill, I’m still having to walk up those, it feels like it’s an issue freeing up energy for my cells fast enough. Stamina is not too bad so long as I don’t go too fast.
Looking at my results, the doc will get upset as he’ll only test TSH, see it’s under range and panic. But T4 is near the top and T3 about halfway, so I’m not over medicated.
After all that waffle I’m going to get to the point and ask the questions.
If I tweak my dose by reducing to 6days 100mcg and nothing on the 7th, that will bring my TSH up a bit, possibly to the bottom of the range, yes?
Posts here the last few weeks have suggested that TSH promotes the conversion of T4 to T3, so might this also help boost my T3 levels? That sort of makes sense as last year when I had dire levels of T4 and over range TSH my T3 was relatively normal.
Try it for 8 weeks, see how I feel, get another set of tests??