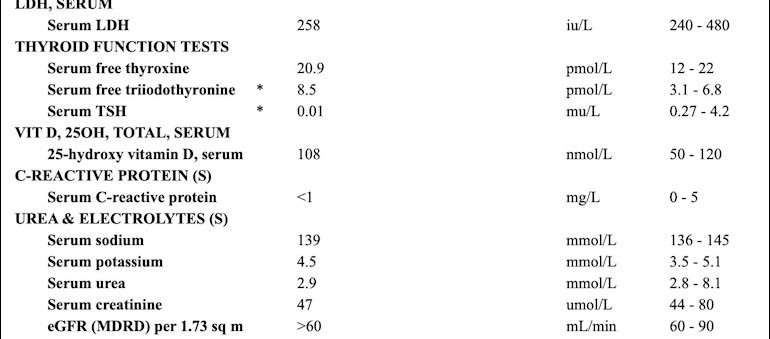
Hi everyone, further to my (rather long-winded!) post yesterday (below), I've just got my latest results, which I've attached. I'm no expert but I'm guessing my FT3 range does suggest I am currently over-medicating? Thanks in advance!
Hello lovely people, I went to see an NHS endo yesterday and he's just called with the results and echoed what I was told by a gyne a few weeks ago - that I may be overmedicating and he's told me to stop taking T3.
I'm currently on 125mg Levothoryxine and 12.5mg of Cytomel.
I'm 45 and have Hashimoto's. I've felt 'under the weather' for as long as I can remember, but for the the last 18 months I've had nausea, sickness, fatigue, aching limbs, sinus problems, dizziness and depression/anxiety. I am single and self-employed and some days I'm so exhausted I'm unable to work, which is very worrying. I can be okay-ish one day, and then barely able to get out of bed the next. I also have flare ups of symptoms that last for around two weeks.
My doctor suspects I may have Addison's Disease based to two low results from previous cortisol tests, and I'm having another blood test next week. However, I am currently on 100mg oestrogen patches, which I have been told will push my cortisol level up, so I'm concerned it won't be an accurate reading.
I did raise this with the endo who told me 'not to worry about it'. He's also told me that if the reading comes back as normal he will draw a line under my symptoms being endocrine-based and discharge me. When I went to see Dr Peatfield he said my adrenals weren't working as they should be, and when I had a private blood test last year my DHEA was low, so it sounds like my adrenals are struggling. But if the result comes back as 'in range' I feel like I'll be back to square one.
Obviously I'm worried that stopping the T3 could make me feel worse, so I'm really conflicted. I can't afford to go privately again so I feel a bit stuck, and any advice would be greatly appreciated!