A general question for those who have got this far in their investigations. It is clear from my fairly short time reading the forum that the practises in various parts of the country vary significantly, despite there being (supposed) national guidelines on the treatment of B12.
I wonder if others have managed to find what their GP or Practice is using if they are not following the NICE or BSH guidelines.
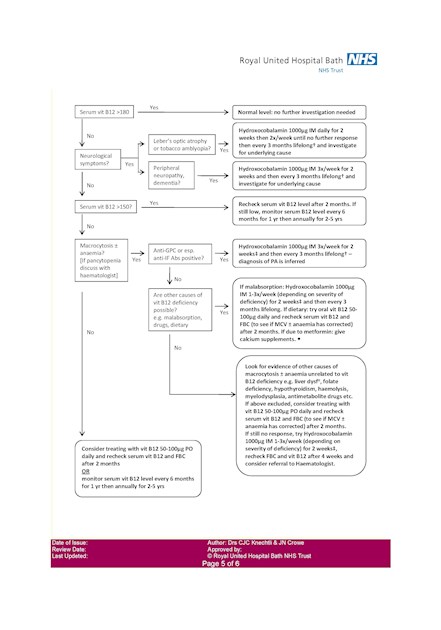
From recent correspondence I've had with my neurologist (based in Kent), she gave me a copy of the attached flow chart, which comes from a Royal United Hospital Bath document - Page 5 of the full pdf available here: ruh.nhs.uk/For_Clinicians/d...
The document seems to have some useful information in it, but the treatment algorithm does not match either of the main guidelines.
In particular:
1. It doesn't recognise any treatment more robust than 6 initial / 3 monthly even where there is peripheral neuropathy or dementia
2. It doesn't seem to consider cases where macrocytosis is not present, yet all the other clinical signs are - (it suggests daily oral supplement of 50-100mcg OR 6 monthly check)
3. It also includes the option to give 1 injection / week for 2 weeks, checking B12 after 4 weeks.
4. It mentions the Schilling test - something that I understand hasn't been available for some time in the UK.
From looking at the references in the document, it appears to have been created in 2010 or not long afterwards, and therefore may be referencing older guidelines and versions of the BNF that have since been updated.
If this is in widespread use, I wonder if it is the cause of so many GPs and/or consultants sticking to the 6/3 treament. Does anyone have experience of it being used elsewhere in the country?
Ironically the further sources of information for patients gives the PAS as a link - and the patient.co.uk page it links to now contradicts the flow chart as it references the more recent guidance.
Interestingly, I found the following on the RUH Bath haematology department site:
How to interpret low B12 results.
Dr Knechtli has just completed a new and comprehensive review of B12 deficiency which will be available shortly on the Haematology Documents page. This document will act as a reference and also contains a useful algorithm for managing these patients.
It's not available yet, but it will be interesting to see if the updated version changes the algorithm to come in line. If so, I wonder whether that will be propagated to everyone who is currently using the old and arguably outdated version.
Any thoughts?
Gavin