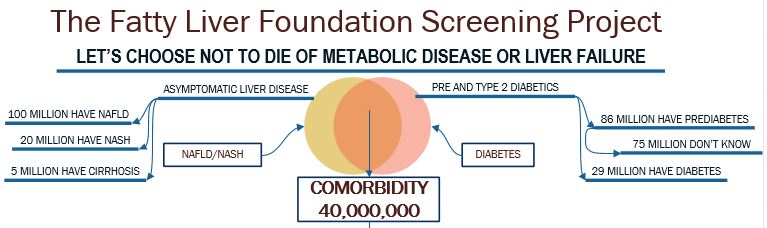
If you think about the co-morbidity illustrated in this image, it is clear that there are at least 40 million Americans who are at some level of risk for developing advanced disease. The question, "WHAT TO DO" hangs there in the face of vast suffering to come.
Studies are coming in as research focuses on liver disease and the challenges that we face. A whole body view instead of organ by organ is becoming more common which recognizes that the liver is so foundational to health that a very wide range of diseases are co-morbid with liver disease. That is a fancy word that means the problems are related.
A good example is diabetes. The high degree of co-morbidity of NASH and diabetes is well known and up to 70% of T2D patients have undiagnosed liver disease. There is a lot of data about the co-morbid nature of liver disease. It may be fair to ask how it is possible for 70% of the diabetes patients to have undiagnosed liver disease, but it is simply due to the fact that absent complications it isn't looked for. If you want to look at the research, here are a couple of links
ncbi.nlm.nih.gov/pmc/articl...
ncbi.nlm.nih.gov/pmc/articl...
It is important to understand that this is related to the standards of care published for the profession and is based upon the fact that there hasn't been enough testing to validate the use of existing tools in a screening mode. If you are interested in reading the guidelines, here is a link to the current document.
onlinelibrary.wiley.com/doi...
Since the policy is that we probably should screen but can't prove it, what is the next step? It is a classical thought experiment, might it not be better to intercept that disease process before it becomes a fully co-morbid problem? The question then is can it be done? Recent studies by several researchers have shown that Fibroscan is about as effective as MRE in identifying fibrosis at late stage 2 and higher as reported in the material above and is much cheaper.
If we take the result of our thought experiment to be that we can and should divert patients prior to illness, how do we do that? We know that diet is fundamental and it is generally recommended that people eat a plant based diet. A recent review of available studies is of value as it summarizes what we know at this time. Here is a link to an excellent review of current thinking.
fattyliverfoundation.org/r?...
We recommend a substantial surplus of oleic acid as the dietary fat associated with a plant based diet. The study by George ET AL outlines the current situation well, but our view of dietary fats goes beyond these guidelines and recommends that the predominate fat should be oleic acid from extra virgin olive oil. We believe our view is supported by this research among others, but confer with your doctor before making dietary changes as we are patients not doctors.
ncbi.nlm.nih.gov/pubmed/233...
The use of oleic acid yields the most efficient energy production at the mitochondria and is foundational to a healing diet. As a review, here is a link to our diet recommendations.
fattyliverfoundation.org/na...
The solution to the problem posed by the standards of care guidelines is to do the work required to satisfy the standards committee that screening really is worthwhile and it is the mission of the Foundation to carry out this screening study in order to intercept people who are unknowingly developing liver disease and divert them to care through early screening so that they may not develop life threatening illness. For more information, here is a link to an overview of the project.
fattyliverfoundation.org/sc...
We hope you are well.
Wayne Eskridge