It is often said on here and other groups that ultrasound is of no use for detecting/diagnosing endo. This is most likely based on so many ultrasounds coming back clear. However, it is incorrect and potentially harmful for those with endo to be told this. This implies that the scan technology itself cannot detect endo.
Great strides have been made in imaging technology and it is about the training and technique of the operator and not the equipment. Basic sonographers in gynaecology departments usually come from a background of midwifery or radiography and will typically only have level 1 training. This teaches how to look for abnormalities affecting the uterus, ovaries or tubes - so just the reproductive organs. A tell tale sign is when the report only mentions the uterus and ovaries. Sometimes ovarian endometriomas will be found as these are well defined on ultrasound unless very small. This then acts as an endo diagnosis, that being ovarian endo.
Endometriomas are almost always associated with deep rectovaginal endo (severe disease) but these sonographers are not trained to look for it. There is a severe lack here not only of training but of understanding. If a basic sonographer finds an endometrioma they need to know that this is a sign of rectovaginal endo and if someone trained to look for it was called in it could be identified with immediate referral to a specialist endo centre following.
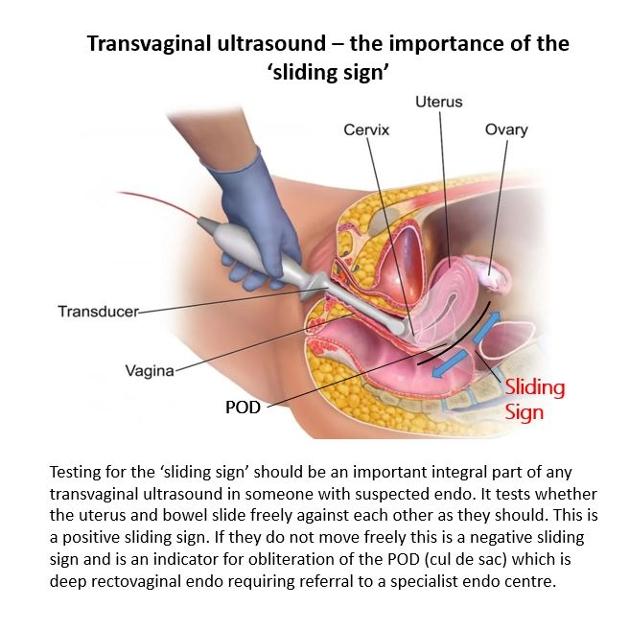
Level 2 sonographers are trained to look for non-ovarian endo and the cardinal sign for rectovaginal endo is a negative sliding sign. This means the uterus and bowel are stuck firmly together and indicates an obliterated pouch of Douglas (cul de sac) which in turn is the classic presentation of stage 4 endo. Sometimes the ovaries will be stuck to the back of the uterus (kissing ovaries) which would be a sign of a frozen pelvis, the most severe form of pelvic endo. Symptoms of rectovaginal endo will most often be left sided (although not always) and lower back pain, leg pain, pain with deep sex, bowel problems, and stabbing shooting pains up the vagina and/or bottom are often typical.
There are some who go on to gain advanced expertise in ultrasound detection of endo but these are usually attached to specialist endo centres in tertiary care or private only. That then becomes a catch 22 - you need evidence of deep endo to be referred to a centre but most of the advanced sonographers are in those centres. The fastest course to diagnosis of deep endo and referral to an endo centre is via a private expert ultrasound which typically costs around £300 for those with the funds.
We understand that BMUS (The British Medical Ultrasound Society) are looking into this. Even without access to an advanced expert in a centre or privately what we need is for all those being referred for ultrasound for suspected endo is a pathway that requires referral to a level 2 sonographer who is proficient in assessing the sliding sign. Dr Susanne Johnson, world renowned expert and educator in ultrasound detection of endo, from Southampton, said in a recent presentation by the BSGE that it is very easy to learn.
We are still some way from scans being able to identify superficial endo that affects just the peritoneum (pelvic lining) and this post clearly is related to deep endo, especially rectovaginal for which ultrasound is the first tool for a definitive diagnosis. GPs should be requesting that a sonographer with the appropriate level of expertise is applied in referrals so don't be afraid to point this out and also to gynaecologists sending you for a scan.
For those with clear ultrasounds done in general gynaecology the first advice would be to obtain a copy of the scan to see if it does indeed report only on the uterus and ovaries. The BMA gives good guidance here but feel free to pm for more detailed guidance.
bma.org.uk/media/2821/bma-a...
You then need to think about whether you might have symptoms of severe endo. Sometimes, rarely, severe disease will be present without symptoms but usually there are typical symptoms and signs. Click on my profile for a detailed post on endo symptoms.
Feel free to pm for access to a list of experts in imaging of endo.
Video by Susanne Johnson:
youtube.com/watch?v=O1IzSOw...
File by Endometriosis Guidance and Information Resource UK (Endorevisited)
 very interesting! It makes sense that elements can be seen on the scan, such as the limited movement, providing a highly qualified person is performing the scan.
very interesting! It makes sense that elements can be seen on the scan, such as the limited movement, providing a highly qualified person is performing the scan.