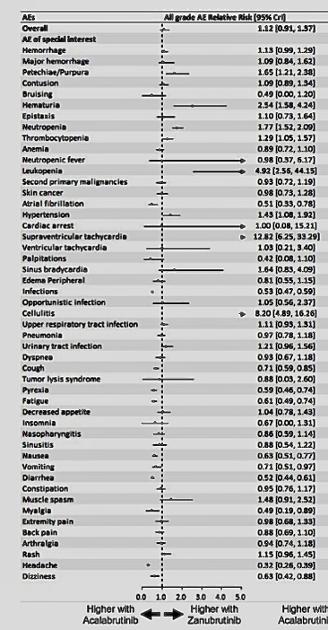
Can anyone suggest why, given the results of a published meta analysis shown here, Zanubrutinib treatment should be preferred to Acal treatment? I understand that these results are not the result of a direct comparative study between the two but on studies of each relative to ibrutinib, and hence that the results are hypothetical or suggestive rather than definitive, but, faced with this exact choice at the moment, I’d like to know which to go for and personally, having had cardiac issues before, I’m leaning towards Acal, mainly based on this graph. Am I being daft? I understand that there’s not much difference in efficacy between the two. Are there any direct comparative studies going on at the moment? Thanks in advance.
Acalabrutinib v Zanubrutinib side effects - CLL Support
Acalabrutinib v Zanubrutinib side effects
For better context, can you share a web link to the page where the graph comes from? If you share the image within a comment, it can be enlarged. Unfortunately, images at the top of a post cannot be enlarged.
Unfortunately, I can’t find the link to the diagram. I believe it was in “A matching-adjusted indirect comparison (MAIC) of the efficacy and safety of acalabrutinib (acala) versus zanubrutinib (zanu) in relapsed or refractory chronic lymphocytic leukemia (RR CLL)” by Adam Kittai, Alan Skarbnik, Miguel Miranda, Alan SM,Jack Roos, Robert Hettle, ...
meetings.asco.org/abstracts...
and was published last year.
Stupidly I took a screenshot but now can’t find the link. Sorry.
Here is a paper (same authors) with a different set of charts (from 2023).
Depending on the size of the image you originally saved to your device for sharing it above, if you share that same chart down here in the comments, we may be able to "click to expand" it. Right now it's just too small to read (because there's no "click to expand" option available in the top of a post.
There is a LOT to unpack about BTK inhibitors, and hopefully more knowledgeable people will jump in. I barely understand it and am not confident trying to explain it. The comparison you listed is for relapsed or refractory (R/R), but isn't this your frontline treatment? Also, I think (again) that it's important to include your 17p marker in this discussion. Context is so important in this very complex and heterogenous cancer.
I’m clearly naive both technically and re CLL! Here’s the diagram again. Any better? I had naively assumed that side-effects would be relatively independent of CLL subtype. Is that wrong? And, apart from being bad news, what exactly is the importance of my 17p deletion? Thanks for your help, neurodervish, and apologies for my ignorance!
I sure understand the challenge in wading thru all the acronyms and new info. It's a lot to take in and can be completely overwhelming. I found youtube videos helped me understand it better. Once I learned the sciency alphabet soup, I started watching CLL specialists doing panel discussions on onclive.com. The videos offer the added advantage of teaching me how to pronounce the new words, so I can impress my doctor. 😀
Here are a couple beginner links you might find helpful:
This video explains a bit more about 17p: youtube.com/watch?v=g5Aa3oK... “Medical Oncologist Dr. Daruka Mahadevan, MD, PhD, provides insight on genetic differences that can be detected in CLL patients. Deletions in specific chromosomes, 11q, 13q, and 7p, can be indicative of dysfunctional DNA damage responses and defective tumor growth suppressors. (A third copy of chromosome 12 is also correlated to CLL.) If levels of these cell mutations surpass a clinically relative threshold, the patient tests positive for CLL. These cell levels are measured and calculated by the FISH test, an NCCN-recommended technique that highlights regions of mutation with fluorescent probes. Over time, clonal evolution can cause alterations in subclone levels, which is why the FISH test is effective at determining the degree of CLL mutations throughout a patient’s diagnosis.”
Another video I've found very helpful is: “Not Your Father's CLL, Dr. John Pagel youtu.be/L1PDNzZaHOk?t=149 It's a bit long, but it gives a wonderful overview of CLL. It's worth noting tho, that it's 7 yrs old. Many new medications have come out since then, especially BTK inhibitors, such as the ones you're trying to decide between. We now have a wealth of new drug options, and even more will become available.
That’s a great message, neurodervish. I haven’t used videos enough and I’m sure your advice here can help others too. I’m very lucky that my own wonderful haematologist does regular YouTube lectures and Q&A sessions but I haven’t looked further. The trouble is that I only see my CLL specialist every few months for a short visit so it’s great to have this forum to help educate a bit more. Many thanks for that suggestion. I’ll be on it later!
You're not alone there. Most of us only see a CLL specialist 2 to 4 times a year. I'm lucky to live in a state with 2 specialists, but these people are spread very thin. There are people who have to fly out of state to see specialists. While reading is worthwhile, it can be challenging (especially when you're still learning). But videos help the brain process this new information on more levels—visual & auditory.
Yep. I have a 200 mile return drive to see mine. There seems to be a world shortage of haematologists! We’re going to try a video meeting next time. Will that be adequate? Better than a phonecall anyway.
Watched these 2 videos you recommended - excellent. A great way to learn. Also watched the good video advertised elsewhere in this forum today detailing the latest advances in treatments healthunlocked.com/redirect...
I feel much more informed today. Many thanks for your help. And good wishes.
can you see the charts from the link? it's formatted differently
Yes, I can see them but I don’t understand them! Thanks and sorry, cyclist 123. Can’t distinguish the plots on the left graph and can’t see any Zanu info on the right. What’s the bottom line? The bottom line for my comparative plot was:
“Results: After matching, the effective sample size of acala was 99 (66.6%; 65% male; median age 66 years). 12- and 24-month INV PFS are shown below. The MAIC hazard ratio (HR) for INV PFS is similar for acala vs zanu (HR 0.90, 95% CI 0.60-1.36). The risk of having grade ≥ 3 AE (OR
0.66, 95% CI 0.41-1.05), atrial fibrillation (AF; OR 1.32, 95% CI 0.56-3.08), grade ≥ 3 AF/atrial flutter (OR 0.60, 95% CI 0.12-2.89), grade ≥ 3 hemorrhage (OR 0.61, 95% CI 0.19-2.03) or an AE leading to discontinuation (OR 1.14, 95% CI 0.61-2.13) was similar with acala vs zanu.
The risk of having a serious AE (OR 0.61, 95% CI 0.39-
0.97), hypertension (any grade: OR 0.18, 95% CI 0.09-
0.37; grade ≥ 3: OR 0.22, 95% CI 0.09-0.54), any grade hemorrhage (OR 0.54, 95% CI 0.34-0.87) or an AE leading to dose reduction (OR 0.30, 95% CI 0.14-0.67) was lower with acala vs zanu. Conclusions: Acala and zanu have a similar efficacy in patients with RR CLL, while acala has a lower risk of grade ≥ 3 hemorrhage, any grade and grade ≥ 3 hypertension and dose reduction due to AEs vs zanu. Limitations of MAIC analyses mean the results should be viewed as hypothesis-generating.”
In summary, this MAIC showed that, when matching on patient
baseline characteristics known to be prognostic and/or predictive of
INV-PFS, acalabrutinib and zanubrutinib have a similar efficacy in
the treatment of R/R CLL when evaluated using INV-PFS. The risk of
having AEs was broadly comparable between acalabrutinib and zanu-
brutinib, except for having an SAE, any grade and grade ≥3 hyperten-
sion, any grade hemorrhage, and dose reduction due to AEs, which
were lower with acalabrutinib. A strength of our study was that it
followed the published National Institute for Health and Care Excel-
lence guidance on MAIC methodology (DSU TSD 18). 1,6 ALPINE and
ASCEND also had very similar inclusion criteria, study design, and
patient characteristics. This was highlighted by the fact that the
matching led to a small reduction in ESS and there was little differ-
ence between the acalabrutinib results before and after matching.
I would suggest that the differences between acalabrutinib and zanubrutinib provide the option for BTKi choice to be influenced by how the differences in side effect risk factors best match a specific patient. They are both good choices with significantly lower risk of adverse long term cardiovascular events and are much better tolerated than ibrutinib. Clinicians were concerned at the large proportion of patients quitting ibrutinib, not because it wasn't working, but because patients couldn't tolerate the side effects, despite most of these reducing over time, with the notable exception of the risk of developing high blood pressure.
Note: in the attached graphic, the ideal BTKi would have one large red circle covering B-cell BTKi (i.e. high effectiveness) and no (off target) red dots showing elsewhere.
Neil
Thanks Jammin_Me. I’m a bit of a dinosaur so forgive my lack of computational skills. I reverted to the original screenshot and got this. Is it any more visible?
Open image, right click on image and open in a new tab, then it can be zoomed up.
I think the key events here are AFib and Cardiac Arrest. For AFib Zanu is 0.51 against Acala and for CA it's evens. For grade 3 or higher Zanu is still better than Acala for AFib 0.61 but for CA it's worse at 1.5.
The important thing is where the little dot is on the line. The long lines mean they don't have much data and confidence in placement of that dot is low with a wide possible range. When the upper range is in the thousands it probably means they had one event.
I'm surprised given the wider number of "off target" responses that Neil posted, that Zanu is better for a lot of things at the bottom of the chart that make it tolerable, the runs, nausea, headaches etc. and some of those have very short lines meaning very high confidence.
Peter.
Thanks again, Peter. Apologies for being so thick. You’ve given me the necessary ‘lightbulb moment’ by highlighting that the horizontal lines, some with arrowheads, are representing uncertainty ranges and not, as I’d previously imagined, magnitudes or intensities of side effects! What a clown. So that totally changes my interpretation of the schematic. The previously conceived interpretation that most of the arrows were showing Zanu is worse for most things is already in my bin. They are pretty equal. I guess I should let my CLL specialist advise. I was on an ACE inhibitor for blood pressure reduction and one study of Zanu apparently featured 7 sudden cardiac deaths, all in patients taking ACE inhibitors. I have now come off ACE inhibitor firstly because they gave me a cough, a common side effect, but secondly because I don’t fancy sudden death much. 😉🤣 Though, when you think about it, it’s maybe quite a desirable way to go! But maybe not quite soon!
Many thanks for teaching a retired scientist who spent his career measuring and interpreting radioactivity, a random process always measured with significant uncertainty limits or error bars, to remember the old fundamentals, even in this new unwanted world of medical data.
Cheers!
Agree that using the AE horizontal line or confidence interval (CI) helps. The dashed vertical line where the relative risk = 1.0 is sometimes called unity.
If the CI crosses the dashed vertical line, then there is NOT a statistically significant difference between treatments.
As Skyshark notes, a long CI suggests either an AE that rarely occurs and/or no difference between treatments. As a result, those AEs with a long or broad CI that cross the unity line are probably least helpful for decision making.
Thanks julius. Makes sense. And I guess the uncertainties on the Zanu side are often greater because it’s a good bit more recent than Acala so less data.
Further to julius_the_cat 's reply below, healthunlocked.com/cllsuppo... the important column in highlighting what you really want to avoid, is the right hand column showing the more serious Adverse Events (those >3). This is why the lines are longer in this column - there are thankfully a lot less serious adverse events than the all grade averse events in the middle column.
We need more data.
I have been on both of them. I started with Zanubrutinib & was so amazed at how fast it worked. I had a large neck lymph node for 10yrs & it disappeared in 3 days on treatment. However full dose was too strong for me.
I had 2 episodes of chest pain prompted by a 60min Bike Workout. I had Pleurisy 13 days on full dose Zanubrutinib ‘Bibasilar Subsegmental Dependent Aetectasis’ but left untreated-> Left Pleural Effusion Pneumonia vs Aetelectasis 48hrs later but still under treated with just steroids & no antibiotics.
I was then put on Acalabrutinib 1/2 dose for 10.5 weeks but the untreated infections had my chest cavity swelled up with pain & pressure. I felt palpatations but I blame it on the infection. The ER, Oncologist or 2 Pulmonologist would not order antibiotics for me with an extensive Asthma History where I cardiac arrested 3X before 10yrs of age.
Anywho I got a 10 day dose of antibiotics. I could only tolerate 1/4 dose of Zanubritinib over 3 months while my heart & lungs healed. I found a CLL Specialist & she had her Pulmonologist & Cardiologist clear me. Then we increased to 1/2 dose & now my labs are normal. Hgb 9.8->12.5, Plts 76->103 & WBC 81->9.8. Platelets are lagging & so is my neutrophils & I am back to working out🙌🏾
I prefer Zanubrutinib since its the last covalent BTKI released Jan 2023 & they worked out the bugs. No massive headache & least likely for cardiac issues. I feel its very strong so the dose modification capability impresses me. One size doesn’t fit everyone. Acalabrutinib works well, just the headache for 2 weeks is a bit much especially since I don’t do caffeine & it didn’t work as effectively as Zanubrutinib for me. They are both great choices tho!!!
Thanks for your personal experience, CoachVera55. You’ve had quite a rollercoaster but great to hear that you’ve got things sorted. You say Zanu has less cardiac side effects and that’s why I put the original graphic and question on. Just a pity noone can read it! 😂 But, to me, that diagram says the opposite, i.e. it seems to show that Acal may well have fewer major cardiac risks than Zanu. That’s what I wanted to find out.
Best wishes to you in this tricky balancing act! We’re just lucky to have these options.
FYI: When I was diagnosed in 2018, I was enrolled in the last phase of trials for Zanu, but was in the control group which received conventional Bendamustine/Rutuximab (sp?) infusions. My oncologist seemed quite positive with the results he was seeing for Zanu. However, when I came out of remission and needed to start therapy again this year, he chose Acala + Ventoclax. I never questioned him about why he chose Acala vs Zanu, but I will if I get a chance. I usually only see the Nurse Practitioner.
Maybe it’s best not to tie ourselves in knots, like I’ve been doing, trying to work out the best balance of the scientific parameters for every option? Maybe we should just trust our CLL specialist haematologist? I guess we’re all different in how much we want to be involved in the nitty gritty. All different too in how we react to every treatment!
Good luck with your A&V.
Keep in mind this key detail from the paper:
FUNDING INFORMATION
This work has been funded by AstraZeneca, USA.
👀
Hi Fogey, I started acala on Jan/23 and was doing great until July/23 when my platelet count dropped to 26 from 95. I was taken off acala And put on prednisone to try to increase count to over 50 and then given rituximab to get platelets up. I was put on 1 - 100mg caps of acala daily and then switched to 2 - 80 mg of zanu in Jan/24. I am now on 1-80 mg of zanu Long story short is I was told by my Oncologist that Acala and Zanu are pretty close but you have more options with dosing with Zanu. Hope this helps. Rrriver