My husband had a bad pneumonia and admitted to the hospital. He has been having neutropenia and low WBC at 1.7 for several months. The heme-onc physician was scheduled to see him in November but because of the bad fever and tremors, we went to the ER. They admitted him and loaded him with antibiotics the WBC went down to 0.8, the doctor decided to give him neupogen GCSF on the 23 October. The 24 October,WBC still low and the peripheral smear showed several blast cells. The 25 October, the bone marrow had been collected and send out for testing. The doctors apparently have no idea that GCSF was given to him prior to collect the bone marrow. The flowcytometry came back indicated Myelobast present. But the still waiting for more genetic testing. My question would be if the GCSF affected the results of his bone marrow? And how. I would rather them do another bone marrow biopsy to confirm that. Please help shred some light to the issue. Thank you so much.
Neutropenia again: My husband had a bad... - CLL Support
Neutropenia again
G-CSF (Granulocyte colony stimulating factor) is a (glyoco)protein that stimulates extra neutrophil production, so the synthetic drug Neupogen will change the steady state of your husband's bone marrow - it's what the drug is designed to do! en.wikipedia.org/wiki/Granu...
There's a range of G-CSF drugs with varying capabilities, including how long they're effective (it takes about 10 days for production of neutrophils from stimulated stem cells).
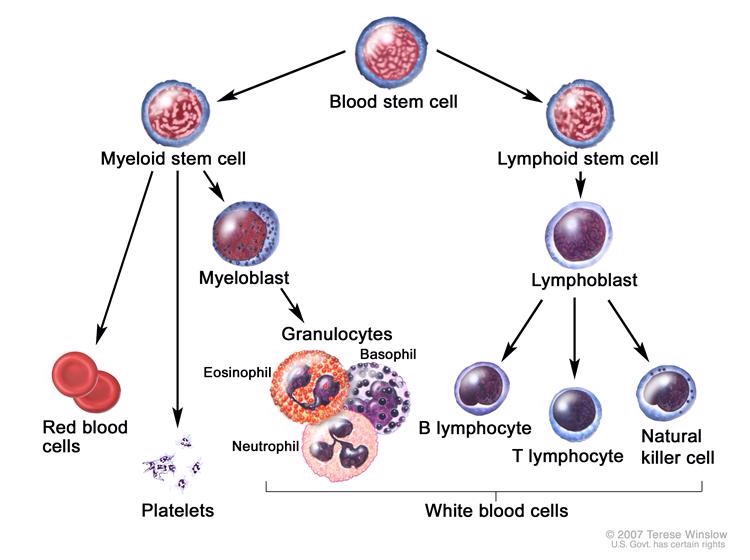
Myeloblasts are precursors of neutrophils, so it would be surprising NOT to find them in your husband's bone marrow biopsy after a G-CSF injection:
en.wikipedia.org/wiki/Myelo...
(I've taken the liberty of editing your post to include a diagram showing how blood cell lines develop. In it you can see how neutrophils develop from Myeloblasts, which come from the Myeloid Stem Cell line.)
So in my non medically trained opinion, you are quite right to suspect the validity of your husband's bone marrow results and should raise this with his medical team.
Neil
Thank you Neil, I asked that question to his doctor today. He is transferred to the higher level of care in the area. Unfortunately, it is weekend, all the specialist physicians are not there. I don't want them to start chemotherapy until we 100% sure that my husband has leukemia. The physician seems to want it done right away. I don't really want to...what is the pros and cons? Please help us make this decision...thank you all
Jan, sorry I was misled by your title - the 'again', made me incorrectly assume you'd been a member for some time and not recently joined.
You are right to question your husband's treatment - possibly for several reasons in addition to the possible confusion caused by the G-CSF administration on the 23rd.
It would help if you provided more details, primarily where you are and how old your husband is. You might like to edit your post (or I can do it) to make it private to this community - by selecting the 'v' at the bottom right of your post and selecting 'Edit'. Otherwise it can be found by an Internet search.
You've joined a community supporting those and carers of those with Chronic Lymphocytic Leukaemia/Small Lymphocytic Lymphoma (CLL/SLL) , which is just one of the more common Non Hodgkin Lymphomas (of whichy there are many) and CLL/SLL more common in older people. (Median age at diagnosis is early 70's, but we have some members in their 20's and 30's.) Because CLL/SLL disease is chronic and incurable, treatment is not recommended until absolutely necessary. For instance, I was diagnosed at stage 4 nearly 7 years ago with the SLL form of the leukaemia/lymphoma, with a low neutrophil count like your husband, but a normal lymphocyte count. (My neutrophil count was half your husband's at 0.4 and I've never been given G-CSF - but then fortunately I haven't had pneumonia either. I also haven't yet had any treatment for my CLL/SLL).
So, firstly, depending on the leukaemia type, treatment may or may not be required immediately for your husband.
Secondly, while some drugs work for a range of different leukaemias, your husband's responsiveness to chemotherapy will depend on having the right drug for his particular blood condition - assuming he even has leukaemia/lymphoma! (and there are non-chemotherapy drugs with less side effects and greater effectiveness than chemo treatment nowadays.)
If your husband has an acute leukaemia/lymphoma, then I expect treatment should be started fairly promptly - it depends on how aggressive the disease is and how his blood counts are holding up - primarily his red blood cells and platelets (which can be supported by transfusions if necessary while the correct diagnosis is made). (But again note that I'm not medically trained and I haven't read much on leukaemia/lymphomas outside of CLL/SLL.)
There's a standard test used to determine which leukaemia/lymphoma a patient has - or whether they have one at all - called Flow Cytometry. It can be done on a blood sample or a bone marrow biopsy - or even a lymph node biopsy for that matter. In my non-medical opinion, your husband should have had that test done to find out what he has and then his outcome will be best served by being checked by a haematologist specialist in blood disorders - ideally one that treats patients with your husband's specific blood condition.
There's another (newly starting) community supporting those with acute leukaemias: healthunlocked.com/acute-le... Perhaps that might be more appropriate for your husband.
Let us know how you go,
Neil
Hi Neil, I'm 65, male, diagnosed 3year ago w/ CLL but probably had it at least 6 years. I have no symptoms per se, my blood counts are reasonably good, have the good genetic markers, I feel about as good as a man my age would. Cycle 10 miles most days but my neutrophil count has drop from normal range to current level of .5 during a course of one year. They want to start treatment. I'm curious as to why you haven't been put on treatment considering your neutrophil count is so low. Thanks in advance.
Also I have no other health issues other than having quite of few skin cancers removed during the past 5 years.
Welcome to our community - I see that you have just joined.
Quite simply, neutropenia is not a recognised reason to start treatment - see:
healthunlocked.com/cllsuppo...
In fact, pretty well all treatments cause (or worsen existing) neutropenia - at least until the bone marrow begins to recover. Eventually treatment should address your neutropenia, but until it does, you'll be at greater risk of infection.
Last year my specialist prescribed regular G-CSF injections after I was admitted to hospital with febrile neutropenia, and I've been having them now for nearly 18 months. I'm into my 11th year of neutropenia and my specialist didn't prescribe the injections earlier, because they weren't sure of the long term use repercussions.
I recommend you seek a second, independent opinion. You haven't shared where you live, but if you are in the USA, you can arrange for a free video consult with a recognised CLL specialist through the CLL Society's Expert Access Program: cllsociety.org/cll-society-...
Neil
Thanks for your response. Addressing the neutrophil count was my line of thinking as well. When I had this recent prognosis, since my numbers have been going well up to this point, I wasn't armed with questions with my onc. But after doing some research I'm perplexed as to why she suggested treatment with Imbruvica, due to the effect it has on neutrophils. This prognosis was given following a recent bone marrow biopsy, so possibly there are other factors that went over my head during my visit earlier this week. I do have an appointment a week from Monday with another oncologist for a second opinion and I'm trying to arm myself with more information about various treatments. I'm in the USA
I'm pleased to hear that you have arranged for a second opinion, because nowadays bone marrow biopsies are rarely done unless there is something rather unusual happening with your blood counts. Perhaps that was the case. For your second opinion are you able to find a haematologist or at least a haematologist-oncologist? Oncologists tend to specialise in solid tumours and you want a specialist in blood cancers, ideally one who sees lots of CLL patients, so they can find the time to keep up with the fast changing treatment world for CLL. The CLL Society maintains a list of specialists recommended by those registered with them here: cllsociety.org/toolbox/cll-...
Neil
