Here is the latest PSMA scan results. Looks like tumors continue rising up the spine to the base of my skull. as of six weeks ago--probably worse by now. Currently on Xtandi half dose and Orgovyx but PSA continues to rise. What the heck are my options? Kishan at UCLA says too much SBRT over last five years to try anymore. (5 times now) Also completed Eclipse Trial last year and Provenge to no avail. PSA now up to 6.7 and going up a point every month.
PET/CT TUMOR IMAGING OUTSIDE FILM REVIEW
DATE: 9/26/2024
DATE OF OUTSIDE PET/CT: 8/19/2024
DATE OF INTERPRETATION: 9/27/2024
PROCEDURE: DICOM files of an outside PET/CT were uploaded to
PACS and reviewed on a multimodality viewing station.
Quality of outside studies cannot be assured, nor technical factors
controlled. Quality control can only be exercised on a locally performed
study.
CORRELATION: None
COMPARISON: PSMA PET/CT dated 3/5/2024
CLINICAL HISTORY: 72-year-old male with history of oligometastatic
prostate cancer status post multimodal therapy. Between PSMA PET/
CTs on 3/5/2024 and 8/19/2024, he was started on enzalutamide and
received interval SBRT to L rib, R femoral head, and R iliac on
5/15/2024.
ONCOLOGIC FINDINGS:
History of metastatic castrate resistant prostate cancer status post
prostatectomy and radiation therapy with:
1. More than 10 new skeletal lesions with mostly intermediate to high
PSMA activity. For example:
* C4 vertebral body without clear CT correlate, SUV max 11.6 (4-117)
* Left scapular spine with underlying sclerosis, SUV max 15.7 (4-151)
* Right clavicle with underlying sclerosis, SUV max 10.4 (4-152)
* Right transverse process of T6 with underlying sclerosis, SUV max
8.4 (4-203)
* Base of skull lesions with low PSMA activity including at the clivus
with underlying sclerosis, SUV max 3.9 (4-77).
1. Right retrocrural lymph node with low PSMA activity, SUV max 2.4
(4-277).
2. Mild bilateral gynecomastia. Left breast gynecomastia is associated
with low PSMA activity, SUV max 3.1 (4-222).
3. Previously treated areas of bony metastases remain without
associated PSMA activity, including the right femoral neck.
ADDITIONAL FINDINGS:
PET:
Physiologic 68Ga-PSMA-11 uptake is noted in the lacrimal and salivary
glands, nasopharynx, vocal cords, gastrointestinal tract (especially
duodenum), spleen, liver, both kidneys, ureters and the urinary bladder,
and testes.
For SUV reference:
SUVmean/max parotid/salivary gland 13.6/18.7 (4-93)
SUVmean/max right hepatic lobe 4.8/5.8 (4-262)
SUVmean/max descending thoracic aorta (level carina) 2.3/2.5 (4-199)
PSMA-expression score*:
High (3): "e SUV parotid/salivary glands
Intermediate (2): "e SUV liver
Low (1): "e SUV blood pool
CT:
HEAD AND NECK:
Atrophic thyroid.
CHEST:
Lungs: Unchanged bilateral lower lobes reticular scarring and
atelectasis.
Lymph nodes and Mediastinum: Ovoid calcified lesions in the anterior
mediastinum, stable.
Pleura: Left upper lobe calcified pleural plaque, unchanged.
Cardiovascular: Mild to moderate atherosclerotic calcifications of the
thoracic aorta and coronary arteries.
ABDOMEN/PELVIS:
Liver: Stable punctate calcification in the caudate likely represents a
prior granulomatous disease.
Gallbladder and bile ducts: Unremarkable.
Spleen, pancreas, adrenals: Stable punctate calcification in the spleen
likely represent prior granulomatous disease. Unchanged mild
prominence of the main pancreatic duct.
Kidneys and ureters: Atrophy of left kidney. Stable left renal lesions,
previously characterized as simple appearing renal cysts. Mild left
pelvocaliectasis without frank hydronephrosis.
Bowel: Scattered colonic diverticula.
Bladder and reproductive organs: As above.
Lymph nodes: Unremarkable.
Peritoneum: Unremarkable.
Vessels: Mild to moderate atherosclerosis.
Abdominal wall: Postsurgical changes in the anterior abdominal wall.
Status post bilateral inguinal hernia repair.
MUSCULOSKELETAL:
As above.
Multilevel degenerative changes of the thoracolumbar spine.
PET-CT body scan image import Date of Exam: 8/19/2024 Page 3 of 3 •
Chronic rib fractures involving the right posterior fifth and sixth ribs.
Retention sutures in the left proximal humerus.
Stable L5 spinous process hardware in place.
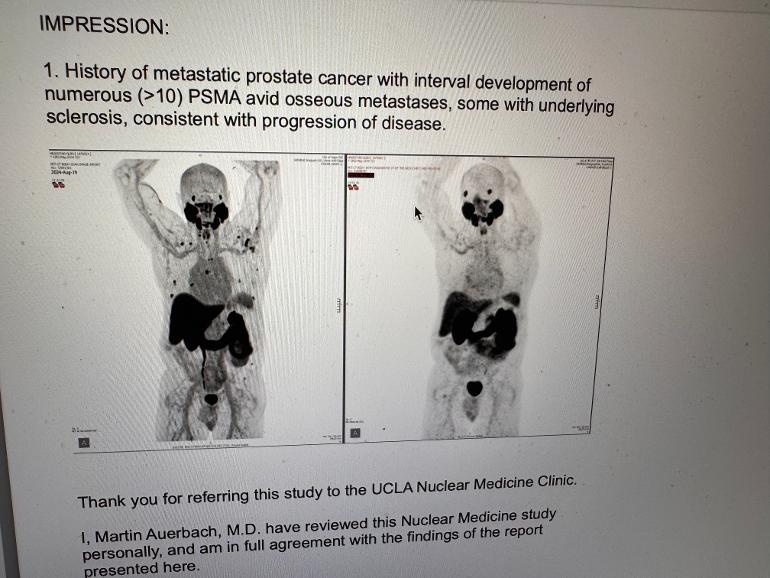
IMPRESSION:
1. History of metastatic prostate cancer with interval development of
numerous (>10) PSMA avid osseous metastases, some with underlying
sclerosis, consistent with progression of disease.