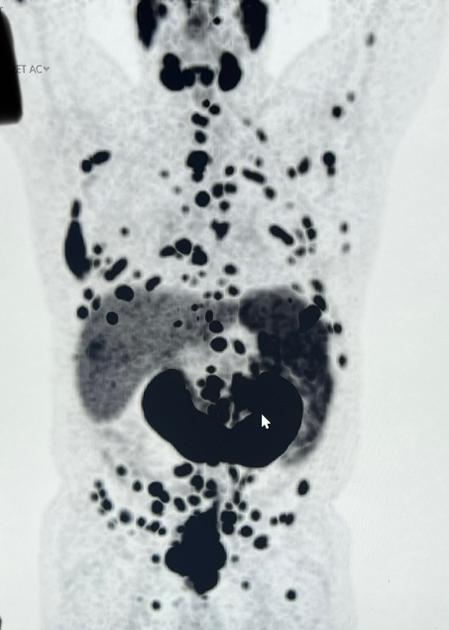
Howdy all. Let me give you a little back ground. I was having some “back” and stomach issues in June and all of July into August. Blood work looked fine, a mass was seen in CT scan near my rectum and lymph nodes in back were swollen. I work in Europe some and traveled for work. My PSA came back at 166 then retest in Europe at 233. Was told of a clinic in Munich that could get me a PSMA right away. They ran blood tests today, seem okay. The PSMA shows that I do have prostate cancer that spread to wrap around my rectum. At least one lymph node is infected (probably more) and a bunch of lesions on bones from higher up on my chest down to my pelvis. I believe I have an MRI tomorrow and a biopsy on the prostate cancer. After that a course of action will be mapped out. This is all coming out of pocket (I am hoping that insurance (BCBS) will reimburse…we shall see). I believe they will remove the prostate and tumors via a “da Vinci” machine later this week or early next. The reason for staying here was the speed at which all of this could be addressed and it seems to be a wise course of action. My question, anyone with a similar diagnosis? Treatments? Suggestions? I’m 53 and healthy otherwise. I’ve attached a photo of the PSMA today. Some of the dark areas aren’t cancerous, just fluid or normal organs (all of which were said to be fine). Thanks so much!
New to this…just saw my PSMA - Advanced Prostate...
New to this…just saw my PSMA
Hi CW, looks like you are well place for Lu 177 if you are already in Germany. I am sure that one of the knowledgeable members will get in touch soon. My husband used Docrates in Finland and they were excellent but I am sure there are many good places close to where you are currently.
Thank you for the info! Yes, they do seem to be on top of things here in Germany at least. Wishing you husband much continued success!
The Technical University of Munchen (TUM) has pioneered a radioligant detector that can be attached to one of the DaVinci's arm. Prior to surgery, the patient is injected with the same radioligand as the PSMA PET you had and so with the aid of this sensor (there was an earlier sensor that worked with Techtenium - but the new one is more specific) the surgeon is actively guided to dissect cancer invaded lymph nodes. The Germans and notably TUM are at least 5 years ahead of the US in novel PCa treatments. Profit from being there.
The therapy used for men in your situation is called "triplet therapy." You can read about it here:
prostatecancer.news/2021/05...
You should not have a prostate biopsy. They will not remove the prostate or tumors.
Having heard that was an option before the diagnosis, I jumped the gun. No removal. Why not have the biopsy? I have heard that they go through at the base of the penis I believe. Can it cause further complications? Thank you for the info!
Once you know it is metastatic, they can't learn anything useful from a prostate biopsy (transperineal or transrectal) that you don't already know. Triplet therapy is the next step - you know everything you need to know to do it.
Wont somatic testing of the biopsy sample ,be useful, to find significant mutations that may be actionable by immunotherapy.
I may be incorrect in saying that your biopsy may return useful information. For example, let’s say that the tumor(s) within the prostate are not invasive to the neurovascular bundles. In such a case (I’m guessing) one could go with brachytherapy and destroy tumors thus sparing the neurovascular bundles. The bundles affect erection capability, so sparing them is likely to be a very +, or it would be for me. Additionally, immunotherapy was mentioned. The cores can be genomically analyzed. Some types of CA are very amenable to immunotherapy and some are extremely resistant to immunotherapy. If, for instance (and I think this is rare) you have a type that is amenable to immunotherapy, it can literally be a magic bullet, not only in the prostate but elsewhere, such as distance mets in the bone. So, biopsy may, in your case, still be a wise move. Ask many questions.
Yes, they can and (IMHO) really ought to do prostate biopsies via perineal. My take is that via the rectum there is way too much potential for sepsis. My urologist said: “biopsy via rectum.” So, I found a new urologist, and had the perineal route, it was a cakewalk, with only minor discomfort for a few days. My first urorogist said: “MRI’s are useless.” The 2nd had me go for a multi-parametric MRI that could be overlayed while he did the biopsy. That made me happy.
There are so many different types of prostate cancer, for instance my Gleason 8, with periprostatic extensions and a PSA of 54 makes me treatable by a fairly narrow group of treatments. In fact, my view is that it’s like the doc is a chef. What’s in the larder is what’s going to get cooked. If there is only chicken and fish, nobody will ever mention rib-eye, but if you read, and read, and read (as many of us do) you might find that in fact, rib-eye is available down the street. It took me a while but I did find that what I wanted was available in Boston, but not in New Hampshire.
And in some cases, you might just find that “that type of product,” will not work for you. I found this when I wanted radiation via Viewray’s MRIdian streotactic device, not for me, as my tumor had gone extra-prostatic.
Over the past month this has been my journey:
Radoc #1 to me: You need Lupron + 35 days of IMRT (radiation).
Then I went to Radoc #2: “You need Lupron + 6 weeks of IMRT + some weeks to the pelvic nodes.
Then at Radoc #3: “Interesting, I suppose we could do IMRT then you could go to Boston and get brachytherapy, and I don’t know about the meds, and I don’t know of a good brachytherapist.
And then today, at Dana Farber (Boston) my path became clear: 1) Orogvyx + Zytiga for September to January (hoping to shrink my BPH prostate from 71CC to ~50 cc, making it more amenable to brachytherapy. (small prostate = better).
My medical oncologist recommended the meds and referred me to a “very good” brachytherapist. My radoc (down the street—nicely) will adjust dosage for first the prostate, starting in January (the meds will stop the Ca for the time being) then the pelvic nodes, then send me to the brachytherapist.
In addition, I will enter a medical trial (Predict-RT) and/ or get Decipher genomic testing indicating “invasiveness potential, aka aggressiveness.” (If low score I may do the meds only for one year, and possibly drop out of the trial if that suits me) If high-score that would likely make me think twice about stopping.
I loathe the thought of those meds and again IMHO I think Lupron is yesterday’s med (again, my Ca is not the same as yours, necessarily) what is good for you may not be good for me, and vice versa.
So, in fact what was offered at doc #1, then at doc #2, then at doc #3 led me to doc #4. Each time I got closer and closer to a treatment path that I felt comfortable with.
And contrary to what had been suggested as the proper path, I will not have Lupron, and I will have brachytherapy.
I’ll confess that I’ve probably spent 160 hours of reading. And it is quite ok to just find a doc you trust and just go with the flow.
Ask questions, seek 2nd and 3rd opinions, find support groups (as is here, and I suggest “reluctant brotherhood” search online. One step at a time. Prostate cancer is terrible, but it’s so very much better these days than it was ten or twenty years ago.
I disagree completely. The OP already knows he already has metastases, so the Gleason score of prostate tissue (which predicts metastases) is useless to know. The genommics of prostate tissue is different from the genomics of metastases, and is also useless to know.
I'm glad you had localized prostate cancer, but that is not the case for the the zOP and your none of your well-meaning advice applies to him, unfortunately.
Might we agree to disagree?
"The integrative genomic profiling of prostate tumors has provided comprehensive information and novel discoveries which improve our understanding of the disease. A number of mCRPC harbor clinically actionable molecular alterations, including changes to DNA damage repair pathway and PTEN/PI3K signaling. The genomic alterations of TP53, RB1, AR, and cell cycle pathway are associated with poor clinical outcomes, whereas SPOP mutation is associated with better clinical outcomes. Several genomic profiling tests are emerging to identify patients who could benefit from targeted therapy. Thus, the genomic profiling of prostate cancer provides useful information for diagnosis and treatment in this new era of precision medicine."
As far as advice, I do not give specific advice, I'm am not a Practitioner, nor a specialist. And if you read what I wrote the only "general advice "in my post is as follows:
"Ask questions, seek 2nd and 3rd opinions, find support groups (as is here, and I suggest “reluctant brotherhood” search online."
My cancer is not the same as his, and neither is yours, nor anyone eases. 99% of prostate cancers are adenocarcinomas, yet there are squamous cell, sarcomatoid, mucinous, small-cell and others, and it may be that that a biopsy of some sort is needed to rule the rarer forms out.
I guess you don't understand that there is a difference between germline genomic profiles and somatic genomic profiles of the prostate and metastases. When you educate yourself about those differences, we can agree to disagree, but I doubt you will disagree.
Sage advice indeed - Too many fellow forum members pretending to be Medically Qualified Experts handing out advice . As a retired professionally trained engineer and business executive , and former business owner . My dad used to remark about such monday morning quarterbacks , as follows .
" They know just enough information to be dangerous -- Or - There's not a topic or question these people profess to know about and can come up with an answer to anything ."
Sage advice from my father .. He never swore , but would say about these types .
" They are talking about that stuff that makes the grass grow in Texas ."
Ask your doctors why they are wanting a biopsy....likely for DNA testing to determine more specific information about the type of cancer cells. The biopsy is done via two methods...one is thru the rectum and the other is the peritoneum (space between the base of the penis and the rectum. In the US they give you a bit of Propofol so you won't feel anything or remember anything. Some places still use local anesthetics. Not sure what they do in Europe. Good Luck to you.
Actually there is a third and a fourth type. There is a liquid biopsy where circulating cells are analyzed and there are cases where individual distant metastases might be analyzed.
"A liquid biopsy is a minimally invasive procedure to investigate the cancer-related molecules in circulating tumor cells (CTCs) and cell-free tumor nucleic acids. There is a high consistency between metastatic tumor tissue and matched circulating tumor DNA (ctDNA) or CTCs [44,45,46,47]. Liquid biopsies have the advantage of detecting acquired resistance in prostate cancer [17,48]. In 2016, Ulz et al [16] performed whole-genome sequencing on plasma samples derived from patients with metastatic prostate cancer, and identified driver aberrations in cancer-related genes, including gene fusions (TMPRSS2:ERG), focal deletions (PTEN, RYBP, and SHQ1), and amplifications (AR and MYC). In serial plasma analyses, the focal amplifications were detected in 40% of cases, suggesting a high plasticity of prostate cancer genomes with newly occurring focal amplifications as a driving force in progression [16]. Although ADT rapidly reduces ctDNA availability [49], the emergence of AR amplification in ctDNA is detected during treatment with abiraterone and enzalutamide [50]. Tumor fraction in cell free DNA (cfDNA) correlates with metastatic burden, and the decline of ctDNA can be a promising biomarker for therapeutic response in patients with CRPC [51]. Decreases in cfDNA concentration independently associated with outcome in patients with metastatic prostate cancer who were treated with PARP inhibitor olaparib (HR for OS at week 8, 0.19; 95% CI, 0.06–0.56; p=0.003) [52]."
Thank you for the reply. Yes, that seems to be the consensus. What would the advantage of immunotherapy be? Sorry for my ignorance, but I am totally new to this diagnosis. Many thanks!
Educate yourself : Purchase Dr. Patrick Walsh's 5th Edition " Guide to Surviving Prostate Cancer " All on this forum will agree , money well spent .
It is waiting for me when I get home. Thanks for the suggestion!
Aaa thumbs up to that. After reading this little banter back and forth, I wonder how well the original poster feels about advice received on this site.
I'm personally glad to see that he posted his details and his bio. 🙀
What I am finding as I have first-hand, in person conversations with people about prostate cancer is that a lot of men typically want to hide it. Especially if they've been treated and the side effects are difficult to talk about.
So I try to remember that what we really want to do is be as open as possible with each other. It is a very complex disease and there is no single panacea.
I think the op owes it to himself to sit down with the book and take his time and calmly read through it. In his own way to his own satisfaction.
May we all have empathy and compassion for each other.
From SOC, if the cancer is not encapsulated within the prostate, a prostatectomie is not performed. Since yours has spread to other areas, it makes no sense to remove the prostate.
That is the part I am having a problem understanding. If cancer in. The body, why not go in, get the prostate, anything around there that is cancerous, and then once the majority is out start hitting it all with chemo? What am I missing?
No, this is NOT an understanding problem of yours. You only happen to have bumped on an anti-RP, pro-RT and pro-ADT forum. What you are considering is formally called "debulking" and colloquially "get rid of the mother ship". The logical idea of eliminating the bulk of the cancerous population is not acknowledged here. There are reasons for this, that I will not share as some silly doc's parrots will start jumping on me, Been there, been jumped on.
Hi-
You are receiving way too much information. Some of it contradicting other recommendations. I would follow the advice of Tall_Allen.
Your PSMA scan has other series of images that include the PSMA isotope, in these you should see colors of blue green orange red in the areas where the cancer has absorbed the isotope. Now have you gone over this with the doctor(s). They will show you that you saliva glands, your liver, your kidneys your bladder and the plumbing that connects the kidneys to the bladder will all light up because those areas absorb the isotope or hold urine containing the isotope. But they are not cancerous.You prostate will light up with cancer.
It appears your cancer has widely spread. So your looking at aggressive treatment.
I had my prostate removed at MD Anderson by their top surgeon who said he was going to take it out regardless if any positive lymph nodes were found during operation due to my early age. That was to prevent any additional cancer from spreading. I was 56 years old. 4+3(7). Seminal vessel spread, prostatic spread. PSA 24 on finesteride for 20 years so calculates to about 60 PSA.
This was done in 2017 before they had PSMA scans. I actually was one of about 200 patients that went to UCLA clinical trial to get PSMA scan approved.
So now the PSMA scan has been the Crux of my treatment plan to this day.
I went on 4 months of ADT, then off until could locate PC on PSMA scan in 2019. 5 spots of PC in pelvis, IMRT radiation to whole pelvic and prostate bed. Two years Lupron. Those cancerous location killed
2023 PSA 1.8 Adaptive SBRT to single pelvic lymph node in sensitive area, not radiated during Whole pelvic. PC killed
2024 PSA 0.8 SBRT to single lymph node pelvic.
Will test PSA in October to see results.
For most people the technology exists today to kill much of the PC by various techniques.
While I began at MD Anderson I moved after my Prostatomy to MAYO clinic. Rochester MN and have several hospitals working with me in various states under the MAYO plan.
Interestingly the special software at MAYO urology department had predicted the latest lymph node before it could be seen. It actually predicted another at a earlier state which still cannot be seen. But the point here is it's finding PC well before the PSMA scan you get anywhere else can and that includes other hospitals including very top US hospitals I've been to.
This plan is working for me, debulk, and kill when found, as I had low volume PC compared to yours.
I choose at the time what I believed was the greatest chance of survival and it seems to be working. Nothing is 100% nothing is guaranteed. But remarkable improvements are happing in medicine, which are and will change everything we are doing today, in a very short period of time. Make it your plan to be around to use the new treatments as they become available and make PC something you don't die from.
If I were you and you'll need to get a PC hospital and doctor in the US (after you have treatment in Europe, and Germany has been well ahead of the US by the way)
Get an appointment with Dr Kwon at the Mayo clinic Rochester MN They are well versed in treating cancer at your stage, you don't want to be just written off by other hospitals and doctors.
Good luck
We are at the same boat Sir, I am not metastatic but GS 4+5 which is very high risk. I was diagnosed at the age of 54 now I am 57. I've been taking Zytiga and prednisone for 1 month cause my Psa raised from 0,04 then 0.08 then 0.12 for 3 consecutives months. My prayer go to all Pca survivors. God bless us
If you are new to prostate cancer you can probably not assess the recommendations you got so far. Anyway, let me add some further recommendations.
I would get a biopsy. Then you learn your Gleason score, whether you have ductal or intraductal cancer and the biopsy probes can be used for a genetic test. They will do a transperineal biopsy in Munich to avoid infections.
In Munich they have developed the radioguided lymphnode dissection, but a lymph node dissection makes no sense if you already have that many bone mets.
I would ask them (e.g. Prof. Eiber) if you can get a cycle of Lutetium177 or Pluvicto. This will destroy several of the mets you see on the PSMA PET/CT. You can get that in Munich but not in the US. In the US it cannot be applied that early in the disease course. I got that and it worked well for me with almost no side effects.
It can make sense to radiate the prostate. Not to fight the cancer but when the cancer grows it can cause urethal obstruction, pain and bleeding. You can get that done when you are back in the US and its covered by insurance.
Fantastic advice! Thank you so much.
since you have so many sites would it make sense to biopsy an easy to reach one to check for mutations?
As he is just diagnosed with PCa there will probably not be different mutations in the metastases and the prostate. Later there may be different mutations in different metastases so I prefer the biopsy probes over the biopsy of a single met.
Concurring with Tall Allen-no need for biopsy if it's already spread. There are other possible side effects from the biopsy itself, which you may as well avoid.
Side affects from the biopsy are pretty darn rare. He indicated they were going to do the peritoneal approach which carries even less risk than the rectal approach. Not sure what they do elsewhere but they administered an antibiotic into my IV after my last biopsy which was the peritoneal way while my first two were via the rectum.
Monty Hall Problem, Pick only one out of three doors which contains the top winning prize.
(Great site huh?)
Good Luck, Good Health and Good Humor.
j-o-h-n
I was diagnosed metastatic Stage 4 at age 55, so similar to you. You can confirm with your doctor that you are, indeed, stage 4. If so, your doctor should be giving you the same advice as Tall Allen has done here. A biopsy is quite invasive. A prostatectomy is still surgery. Both come with risk and won't change your treatment plan or prognosis.
I'm now 61 so I've been at this for over 6 years. Treatments are working well to keep the cancer suppressed. I'm relatively healthy and enjoying life. Good luck.
I listened to it. He is not wrong, but you have misconstrued what he said.
1) He argues for germline testing. Germline testing is done with saliva or serum, not a prostate biopsy.
2) He also argues for somatic testing of prostate tissue, when it is available, to help decide if doublet or triplet is necessary. It is often available because prostate biopsies are usually the first step in diagnosing prostate cancer. But for the OP, he already knows he has metastasized prostate cancer, so that step can be skipped. In the OP's case, a biopsy of a met can provide much more actionable genomics than a biopsy of the prostate. Dr. Smith does not discuss this situation, but I feel sure he would agree with me.
That is exactly what he is saying if you listen without confirmation bias filters on. He says there is no reason to use a PARP inhibitor before castration resistance sets in. The OP was just diagnosed, so there is no reason to check for BRCA+ in his prostate. At any rate, the OP can check for germline BRCA with a simple saliva or blood test now. If BRCA+ shows up only somatically, it will certainly show up in his most recent metastases at that time, but not necessarily in the prostate.
:30"At the present time, PARP inhibitors only have a role in mCRPC."
Half of BRCA+ patients are positive on germline, and half are positive only on somatic testing (or cell-free DNA blood testing). BRCA mutations, like all cancer DNA mutations, occur with increasing frequency over time. Genomic breakdown is one of the characteristics of cancer. So it is more likely to find a BRCA-mutated gene in later metastases than in the prostate initially. So what, in your estimation, is the benefit of a prostate biopsy now? If there are no treatment implications, it is awful to put a patient through an unnecessary prostate biopsy.
You don't get to say, ignore what he says on :30 -only listen to what he says on :33 out of context. You mistake his analysis of a convenient prostate biopsy from the ideal analysis of metastatic tissue.
I asked you the question - what is to be gained from a prostate biopsy that can't better be obtained from a somatic analysis of a metastasis?
Since you can't answer my question, you concede that prostate biopsies after metastases have been discovered are useless. Thank you for the discussion.
I have no idea what that means. In baseball, 4 balls is a walk and 3 strikes is an out - "3 balls and strikes" isn't either. And bats are made of hickory, not pine. You keep saying it is your final post, but then you keep making non-sequiturs or insulting remarks. How can I miss you if you won't go away?
LOL- the LA Dodgers currently lead the National League West with a .600 percent. So I guess you are right that we are elite here in LA.
To bring it back on topic - I'll let you think about the question that I posed and you are unable to answer. Take your time.:
What is to be gained from a prostate biopsy that can't better be obtained from a somatic analysis of a metastasis?
I was diagnosed as de novo polimetastatic with distant mets in my spine and neck.
My first medical oncologist professor Richard Epstein like you also believed that I don't need a biopsy and wanted to put me straight on Degarelix ADT injections.
But my first radiation oncologist professor Izard wanted me to perform a biopsy of my Prostate before I start ADT because a prostate biopsy is a common requirement to enter any clinical trial and if you start Degarelix before the biopsy of the prostate your biopsy results are sqrued.
I was aware about all of these and decided to wait couple of months with my treatment because I was an interesting candidate for the "ADT and me" trial for professor Emmett. We wanted to discover how the PSMA expression of all my mets in my bones change after the initiation of the ADT. I had four PSMA pet scans every two weeks starting with the first at the moment of my first Degarelix injection.
It’s not different. You simply refuse to understand. Reading Hobbes (note spelling) makes me elite? I’ll own that then.
Btw- I’m currently reading Aristotle’s Nichomachean Ethics, after finishing Seneca’s letters and all the extant writings of Epicurus. Understanding the backbones of Western Civilization is good grounding for everyone who lives in it.
I would suggest you and Tall-Allen contact Dr, Smith and settle this childish back and forward . I'm sure in the circumstances , he would reply .