It has been a roller coaster of a few months. After a hemi-ablation HIFU In Germany (4/11/19) Alan had a great nadir of 0.19. Men with that kind of result have a 96% chance of not having a recurrence within five years of treatment. It stayed like that for a year and then increased to .80 in May of 2020 and had reached 2.13 last month.
A 3TMRI in July indicated two possible lesions - Pirads 3 and Pirads 4 high grade cancer. (Alan's only biopsy before HIFU showed two small cores of Gleason 4+3 with a small amount of Gleason 4+4 pattern. The two small tumors were T1c's.)
With the rising PSA and supected lesions on July's MRI, Alan got scheduled for a PSMA-PET Scan at Dana Farber on 27 September. No sign of metastasis, but there was a small intensity seen in the prostate. All signs pointed to a recurrence. (BTW this was a Pylarify PSMA PET Scan and was fully covered by Alan's Medicare.)
To rule recurrence out, Alan had an in-bore, MRI guided perineural biopsy at Brigham and Women's last Wednesday (with Dr. Tuncali who has done more than 1,500 of these) and miracle of miracles, no cancer was found in the two suspected areas (it was fibromuscular tissue - maybe scar tissue from the lesions he had removed in Germany?) and another six samples were taken from various parts of the prostate to be sure. All were benign!
Many doctors use the Phoenix definition to assess a biochemical recurrence following HIFU, which would be a PSA of 2.00 above nadir, or in Alan's case 2.19. At his present PSA of 2.13, that is awfully close to that limit, but in the absence of any cancer found on his PSMA PET Scans or MRI Guided biopsy, Dana Farber says there is nothing to treat as far as they can discern.
So Alan has been put back on active surveillance. Hooray! But if his PSA continues its rise and hits 4.00, he will need to go back for more testing. We would like to think he is out of the woods for now (maybe re-growth of prostate tissue caused the PSA rise?) but we are not sure what to think. Any ideas? BTW we were very, very happy at Dana Farber. The oncologist, Dr Choudhury, was awesome.
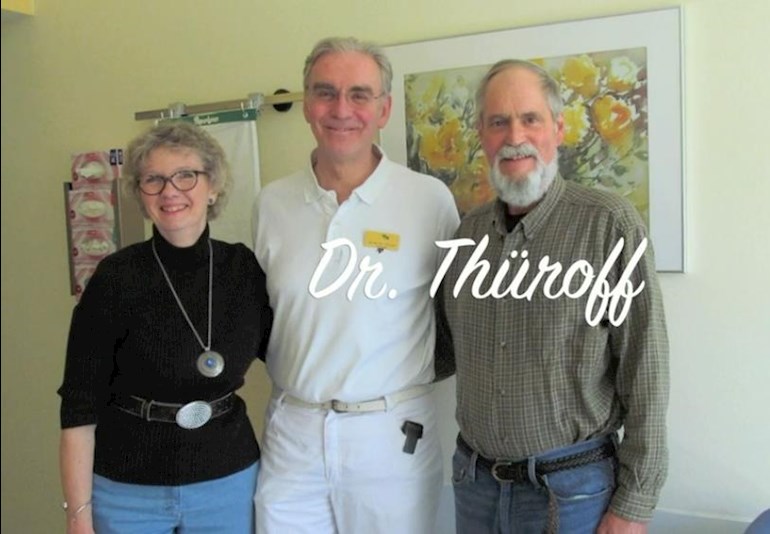
We are seen above with Alan's HIFU doctor (Dr. Stefan Thüroff in Munich.) He practiced HIFU treatments on patients for more than 25 years before retiring last month. He was a wonderful doctor and always considered QOL for his patients.