Based on the above blood test results, the nurse at my health centre has called me in for an appointment tomorrow to talk about the dangers of my suppressed TSH. Has anyone got any advice on how to respond simply, to avoid them reducing my levothyroxine please? I currently take 125mcg 3 days a week and 137.5mcg 4 times a week. I also take 31.5mcg of t3. Many thanks
Suppressed TSH: Based on the above blood test... - Thyroid UK
Suppressed TSH
How did you take this test?
Time of day?
When did you take last dose of Levo & T3 before the test? How much T3?
These are details that will determine of your test is a good picure of average levels or showing false low particularly for FT3.
Your FT4 is only 43% of range, needs to be around 70%.
How do you take your Levo?
Always take Levo on an empty stomach an hour away from food or caffeine containing drinks & other meds. Many people find taking it at bedtime works well for them.
What supplements do you take and what are latest results for vitamins?
You are on a high dose of T3 so your result is surprisingly low at 38% of range.
GPs dont like low or suppressed TSH results. You can use NICE guidelines that state this:
The first paragraph in the NICE (NHS) Thyroid Disease, Assessment and Management guidelines says :
nice.org.uk/guidance/ng145
"Your responsibility”
The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service. It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian. “
is your T3 prescribed?
If yes…by GP or endo
Was last dose Levo 24 hours before test
T3 ….day before test split T3 as 2 or 3 smaller doses spread through the day, with last dose approximately 8-12 hours before test
is this how you did your test
The dosing was done as you said and I buy the t3 myself. Before I added on the t3, I felt awful. I could barely function and now I'm relatively well and my energy levels are mostly good.
So as self sourced T3 …..in order to keep your levothyroxine dose from being reduced you will probably need to see endocrinologist
GP is unlikely to agree to suppressed TSH without endocrinologist overseeing
If anything, you might need small dose INCREASE in Levo
I saw an endocrinologist last year when I was on a dose of 125mcg of levothyroxine and they wanted me to reduce to 100mcg to bring my tsh back up. I wasn't happy about this and the gp agreed to let me stay on the 125mcg. They were aware of the self sourced t3, but didn't think of needed it, despite me explaining it felt better on it.
Ah right.
Then the simple response is, “I take T3–liothyronine. It’s already in my notes. It’s well known to suppress TSH. I discussed this with Dr X last year after seeing the endocrinologist and it was agreed I could stay on 125mcg levothyroxine. I’m well aware of the potential risks of over medication but I’m not over medicated, as my FT4 and FT3 are well within the laboratory reference ranges. I have the capacity to make decisions for myself. I’m really well-informed on this subject.”
And if they try to argue, stick to your guns. Say confidently, “The thing is, TSH isn’t even a thyroid hormone—it’s a signalling hormone to prompt the thyroid to make thyroid hormones and it’s not a reliable marker for those of us who take liothyronine.
Keep your tone matter of fact. Chances are they only know the very basics and your confidence will hopefully cause them to back off.
But in any case, a nurse shouldn’t really be allowed to reduce your dose. I know that’s the way things are now but it doesn’t mean we have to accept it!
Oh, wonderful reply, Jazzw! I'm keeping this post to refer people to when they ask this same question - as they often do! 
Brilliant response! Tells 'em exactly where to put their pipes and how to smoke 'em!
Fantastic reply Jazzw...I'm also keeping it for the next time I get a 'computer says no' call from the duty doc in my practice. Yet another issue with the NHS: even if you get a GP in the know and they are onside with all your treatment, the system will still throw this kind of nonsense up and demand you see whichever GP or nurse is in charge of 'thyroid patients' or just on duty doc that day if the numbers turn red on them.
That said, they are only doing their job and frustrating as it is, there's no point coming across as a screaming harpy and getting oneself described as 'difficult' or, God forbid, 'depressed' or sim, so I really love your polite but firm means of responding. Absolutely textbook. Thanks!
Hi JBL312,
Have you had your pituitary tested? Problems with the pituitary gland may cause a lower TSH. It may be suffering the effects of hypoT or you may have an actual problem with it. You could say that you would like it tested before altering your dose.x
Not sure if this helps but my understanding is that when the body has enough t3 the pituitary senses this and doesn't send the messenger TSH. Hence it gets lower /suppressed and t4 is also quite low again because there is enough t3- the active hormone. Neither your t4 or t3 are actually high enough so a small increase in either but not both, would help any lingering symptoms .
That's a very interesting comment which leads me to wonder whether the pituitary responds to the amount of thyroid hormone in the blood stream or the amount of T3 in the tissues etc of the body (or both)? As a bit of a dummy when it comes to anatomical workings, I would have thought it would be the former (blood) because how else would the pituitary be able to sense the amount of T4 or T3? Can you or anyone else clarify please?
I was under the impression that TSH is produced as a result of the levels of both the T4 and T3 in the blood. And this is just a guess - I think it may play a role in controlling conversion due to the circadian rhythms of TSH, T3 and T4.
The pituitary is thought to respond to the amounts of both T4 and T3 in the blood that reaches it.
It converts the T4 into T3 and then adjusts - more or less adding the T3 from T4 locally converted to the T3 delivered in the blood.
But the precise conversion mechanism is slightly different to other parts of the body.
And the pituitary is ALSO affected by Thyrotropin Releasing Hormone (TRH) delivered from the hypothalamus to the pituitary.
Also any adjustment by the pituitary is not immediate. It doesn't change the TSH level from 10 to 1 the moment enough thyroid hormone is present. Rather, each day it makes a little less TSH until it reaches some sort of balance. Thus it can take some time for TSH to respond fully. And this is a major reason for the argument that adjustments to doses need to be tested after 6 to 8 weeks.
The pituitary (and hypothalamus )are both directly affected by the levels of T4/T3 in the blood . It is the action of T4 and T3 on thyroid hormone receptors in cells in the pituitary (and hypothalamus) which controls how much TSH is released
So TSH is produced as a result of action of T4/ T3 on cells in pituitary tissue ( and on hypothalamus which produces TRH)
So the pituitary reports on how it ( and the hypothalamus) feels about the levels of T4/T3 acting on it's cells by increasing or reducing the amount of TSH it releases..... but the pituitary has no way of knowing how the cells of the rest of the body feel about that level of thyroid hormone.
TSH only tells us how 'satisfied' the pituitary and hypothalamus are .
healthunlocked.com/thyroidu.... tsh-is-just-the-opinion-of-your-pituitary-about-your-dose-but-your-pituitarys-opinion-is-a-bit-warped-once-you-take-thyroid-hormone.
My TSH is very supressed, around 0.005. I take 175mcgs levo a day. My T4 is well above the range, but my T3 is normal. Been like this for many years. No bone problems, no hyper symptoms and feel fine, I impressed on my GP that I feel well on this dose. When I changed surgeries, I impressed on the new doctor that this dose was 'right for me' and these results are normal 'for me'.
Yes I've got to try not to be bullied by them.
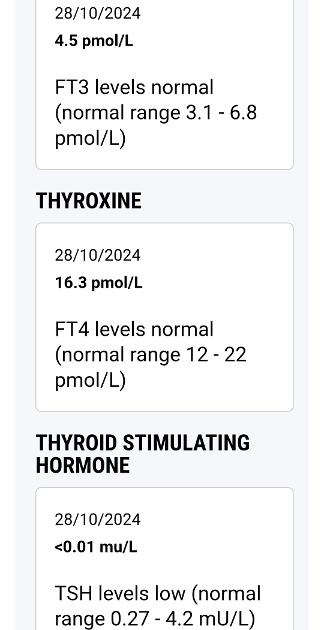
Free T4 (fT4) 16.3 pmol/L (12 - 22) 43.0%
Free T3 (fT3) 4.5 pmol/L (3.1 - 6.8) 37.8%
Assuming you have enough levothyroxine tablets…..try small increase in dose
I currently take 125mcg 3 days a week and 137.5mcg 4 times a week.
perhaps 137.5mcg 6 days a week and 125mcg one day per week
I also take 31.5mcg of t3.
Which brand?
Just to add what @fiftyone has posted above, I am also on levothyroxine only and my TSH has been suppressed since I started levothyroxine in 2003. I take 100 mcg levothyroxine only, my T4 is on top of the range or sometimes slightly over and my T3 is around 60% through the reference range. I had numerous discussions with GPs and endos over the years urging me to lower my dose, which I humoured only once, but no longer, as it just made me ill and did sod all to my suppressed TSH. I went back on the original dose and told them that I cannot function on a lower dose and that it is my risk to take.
I monitor my thyroid and vitamin levels myself once a year, I send the results to the GP practice with the comment 'for your information only and no changes needed'. This is the level I can function best, I have the brain capacity for performing scientific work, I do plenty of exercise & strength training, eat a healthy diet and my glucose and cholesterol levels are picture perfect.
You need to stand firm and defend the levels you feel best on (and with T4 and T3 within the reference range you have a very good defence). They may not agree, but at the end of the day it is your decision and risk to take to have the quality of life you need and deserve.
If they start on the "heart and bones damage" thing, just say that this has been disproved and shall you send them the research papers?
They never even think to keep up with the research!
Hi again, you’ve probably had your appointment by now - was it ok? - but I thought I would come back to your post. I am re-reading Dr Peatfield’s book and have just been reminded that if you have thyroid cancer you are advised to have your TSH suppressed. If it’s ok for a cancer survivor, why is it not ok for you? Your fT3 is in range and TSH has no other effect on the body so lack of it isn’t a problem. It’s your choice at the end of the day. If you want to take what “they” see as a risk then surely that’s up to you. You could say you see living life under medicated as tantamount to a death sentence. It really is like being the living dead!x
most endo's are unlikely to accept that argument Blue_Lagoon( "supressed TSH ok for cancer , so why not ok for you" )
... it's considered worth the 'risk' of taking higher doses to supress TSH in order to prevent TSH from stimulating regrowth of cancer cells in any remaining thyroid tissue.
They consider the risk of cancer regrowth in thyroid tissue overrides the risks of taking slightly too much thyroid hormone .
In patients where cancer is not an issue they will see no reason to allow the 'risk' of supressed TSH.
Also the supressed TSH after cancer policy appears to be changing ... it used to be considered ok/ necessary to keep it supressed for a very long time after thyroid cancer, but nowadays there are papers etc suggesting its only necessary for a limited period ... so even for those who have had cancer, it's not now seen as a justification to keep TSH supressed indefinitely .
Yes I realise it’s to prevent the cancer coming back. As the patient it should be up to you to decide which ‘risk’ you wish to take. Isn't it possible to sign something to say that, as the patient, you take responsibility for your choice of having a suppressed TSH, even if it’s not what your doc would recommend? That lets them off the hook.
There’s always the risk of diabetes, heart attack, stroke, other cancers etc etc with being under replaced. It seems fair to let the patient choose how they wish to shuffle off this mortal coil! 🤣 personally I’d rather take the risk of supposedly being over replaced, feeling well and living life to the full but then succumbing to the consequences of osteoporosis, a fib etc, as opposed to living an awful half life and having it drawn out for years and years! 🤣
I didn’t realise they’re now even saying to cancer sufferers that they should risk their lives again rather than get osteoporosis etc 🙈 what is the world coming to?!x
i agree with you... many of us prefer quality of life now over statistical risks that may or may not happen.
but a patient cannot choose to take the responsibility for prescribing something... the act of prescribing remains the GP's responsibility and so do the professional consequences to the GP.
we have the right to refuse to take a prescription medication for something ..we don't have a right to insist a GP prescribe something when it is against their judgement.
some of us have got GP to write in our notes that we understand the risks of low TSH etc .. which helps , as it lets them off the hook a bit .... but it is in no way binding.... it's ultimately their decision/ responsibility whether to prescribe or not.
Yes. I’m just presenting an argument that could be put forward in our favour that may persuade an endo or GP. I’m not suggesting that people insist on being prescribed something that an endo or GP doesn’t want to do. I just think there’s two sides to it and sometimes they could do with being reminded of the hypo risks which they seem to “conveniently forget”!x
What if several NHS endos take the view that the patient needs a specific dosage of a particular medication? Can a GP in all conscience then deprive the patient of that medication? Surely the GP in that situation is effectively absolved of all liability.
Hi, sorry for the delay in responding. I had my appointment and was told that they levothyroxine should be a lower than what I'm taking and despite making my argument, the gp said they need to liase with the endo (who was also of the same opinion during my last visit). They said they would leave it as it is for now, so I haven't told them that I've increased. As my t3 is self sourced they don't have much to say about that.
I thought an endo “requests” that the GP prescribe and the GP is obliged to listen to them? They are the expert after all so surely the onus is on the endo? The GP referred them in the first place.x
Surely it’s more likely they say no because of the cost of T3 and their budget? Not because they don’t want the responsibility of prescribing because of the risk and don’t want to help their patient.x
I would have thought level of competence is a major factor. A GP cannot be expected to be fully competent in all situations that arise so taking advice from a fully qualified endo must absolve the GP from any liability. On the other hand, Ignoring or rejecting that advice would appear to be a disservice to the patient and amount to incompetence in performing the role of GP.
Do mind me asking. If your on a shared care agreement with T3 between your endo and gp, can your gp just stop agreeing to prescribe at any time they like?