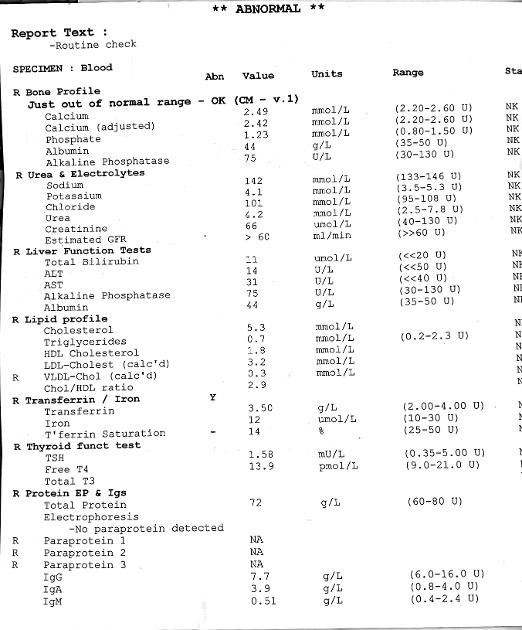
in response to me requesting help to understand my blood test results seaside susie recommended that I get my doctor to check my iron panel. After some persuasion and despite considering all my results satisfactory, she did agree to do this as I am still suffering from fatigue, joint pain, hair loss and I consider some of my results on the low side of normal. I attach the results of this latest blood test which my doctors opinion is all most satisfactory. I have been on a daily dose of levothyroxine of 75 until it was reduced to 50 as I have lost nearly a stone in weight since last October and all other tests for why this has happened have been negative. Though not low in iron my ferritin is still low and apparently I am not converting iron well. There do seem to be many lowish results. I am taking D3 and have increased liver products in my diet and am about to introduce magnesium as recommended. Could I ask what others think.
low ferritin: in response to me requesting help... - Thyroid UK
low ferritin
And here are the rest of my blood test results
I have been on a daily dose of levothyroxine of 75 until it was reduced to 50 as I have lost nearly a stone in weight since last October
Was dose levothyroxine reduced AFTER these results?
Or 2-3 months BEFORE this test
Most hypothyroid patients GAIN weight…..but a significant minority of hypothyroid patients struggle to maintain weight when inadequately treated
These results suggest you need dose INCREASE In levothyroxine
Ft4 is far too low and there’s no Ft3 result
Ferritin is deficient
B12 is insufficient
Folate is insufficient
No vitamin D test results
Was this test done early morning, ideally before 9am and last dose levothyroxine 24 hours before test?
FT4: 13.9 pmol/l (Range 9 - 21)
Ft4 is only 40.83% through range
No Ft3 result
Previous post a month ago on 75mcg showed you were under medicated
And working on improving low vitamin levels
healthunlocked.com/thyroidu...
Are you now on strictly gluten free diet and/or dairy free diet
There are other brands levothyroxine that are lactose free, if Teva doesn’t agree with you
Aristo - 100mcg only
Could take 50mcg and 100mcg alternate days
Or cut to get 75mcg
Glenmark also lactose free. New brand, may not be easy to get
Yes the test was early and last dose of levo more than 24 hours before. The only supplement I am taking is Vit D and I will get this tested as it hasn’t been in this latest NHS test. My doctor knows that I am not satisfied that these results are satisfactory and has agreed to retest in August. My Levothyroxine was reduced at the end of April.
Thank you so much for your clear explanations and recommendations. Sorry to burden you with yet more results but I am at a loss for an explanation of why I feel so yucky other than my advanced years.
At the moment Glenmark not available. There is none available in the network for distribution.
Managing director of an independent chain of chemists in my area telephoned Glenmark yesterday on my behalf as I have 1 tablet left, and this is the only suitable tablet for me.
Glenmark supposed to get back to her. I got it about 2 months ago and seems went out of circulation about then.
51105Scot
I attach the results of this latest blood test which my doctors opinion is all most satisfactory.
Your doctor is saying they are all satisfactory because mostly they fall within their ranges. However, we have to take into account where in the range they fall. Very top or very bottom could suggest something isn't quite right.
Though not low in iron my ferritin is still low and apparently I am not converting iron well.
I disagree with you here (underlined bit) 
Look at your iron panel:
Transferrin: 3.5 (2.0-4.0)
Serum iron: 12 (10-30)
Saturation: 14% (25-50%)
Ferritin: 21 (15-200)
Often quoted here are optimal results according to rt3-adrenals.org/Iron_test_... are:
Serum iron: 55 to 70% of the range, higher end for men - yours is 10% through it's range so is very low in it's range
Saturation: optimal is 35 to 45%, higher end for men - yours is below it's range at 14% - how can your GP say this is satisfactory?
Transferrin: Low in range indicates lack of capacity for additional iron, High in range indicates body's need for supplemental iron - yours is 75% through range so at the higher end
Ferritin: Low level virtually always indicates need for iron supplementation - yours is 3.24% through it's range so is very low
From: cks.nice.org.uk/topics/anae...
In all people, a serum ferritin level of less than 30 micrograms/L confirms the diagnosis of iron deficiency.
So your ferritin is suggesting iron deficiency and your iron panel is showing us extremely poor levels of serum iron and saturation percentage, all pointing towards iron deficiency. Yes, in range which will satisfy your GP but you can see how dire the results are. But even the report says that a ferritin level of 15-50 is an "intermediate resut - consider iron deficiency". How can a GP miss this? Perhaps best to address this now rather than leave it to deteriorate even further and make it harder to put right.
Your haemoglobin and haematocrit are both well within range so no anaemia is suggested, so you appear to have iron deficiency without anaemia.
Comparing these B12 and Folate results with those you posted from your private test last month, they bear no resemblance even taking into account the private B12 test was Active B12 and your NHS test is Total B12, so as you've posted your NHS results here I'll comment on these:
B12: 331 (200-883)ng/L (which is the same as pg/ml)
This is low but in range so will again satisfy your GP. However, many people with a B12 level in the 300s have been found to need B12 injections. So check to see if you have any signs/symptoms of B12 deficiency here:
b12deficiency.info/signs-an...
b12d.org/submit/document?id=46
If you do then list them to discuss with your GP and ask for testing for B12 deficiency and Pernicious Anaemia. Do not take any B12 supplements or folic acid/folate/B Complex supplements before further testing of B12 as this will mask signs of B12 deficiency and skew results.
According to an extract from the book, "Could it be B12?" by Sally M. Pacholok:
"We believe that the 'normal' serum B12 threshold needs to be raised from 200 pg/ml to at least 450 pg/ml because deficiencies begin to appear in the cerebrospinal fluid below 550".
"For brain and nervous system health and prevention of disease in older adults, serum B12 levels should be maintained near or above 1000 pg/ml."
If you have signs/symptoms of B12 deficiency then your GP should treat with B12 injections (or supplements).
So even if no signs/symptoms of B12 deficiency it will be in your interest, particularly due to your age, to increase your level to the top of the range.
Folate: 7.9 (3.1-20)
Your GP will be happy with this and it's certainly not dire, but as we hypos need optimal nutrient levels then it's recommended for folate to be at least half way through it's range. Once B12 has been tested further if necessary, of you have started supplementing with B12 to raise your level, you can then add a good quality B Complex (eg Thorne Basic B) to help raise your folate level and keep all B vitamins balanced.
When taking B Complex we need to leave this off before any blood test for 3-7 days because it contains biotin and this can cause false results.
The only supplement I am taking is Vit D and I will get this tested as it hasn’t been in this latest NHS test.
In post a month ago
Medichecks test
Vit D 67
(,25 deficient, 25 - <50 insufficient, 50-75 adequate, >75-200 optimal
So you don’t need to retest yet
Test September and late January
How much vitamin D are you currently taking
Aiming for at least vitamin D around 80nmol minimum
When was dose levothyroxine reduced to 50mcg
How much levothyroxine are you CURRENTLY taking?
Thyroxine reduced late April from 75 to 50 and the doctor thinks that has improved things but I don’t feel any better. This latest blood test was at 0915 but more than 24 hours from last dose of meds which I usually take at 0500 each morning. To confirm, I am currently taking 50 mic of Almus Levothyroxine which does contain lactose but doesn’t upset me like the Tevo. And at least I have been able to have the same brand for two months now. Following your advise and taking BetterYou D3000+K2.
Suggest you request/insist on 12.5mcg dose increase in levothyroxine
Bloods should be retested 6-8 weeks after each dose change or brand change in levothyroxine
Likely to need further increase in levothyroxine after next test
Avoid Teva
You could see if you can get Glenmark?
Meanwhile working on improving low vitamin levels
2 weeks after starting magnesium
Low folate and low B12 need improving by starting daily vitamin B complex (if not taking this already )
supplementing a good quality daily vitamin B complex, one with folate in (not folic acid) .This can help keep all B vitamins in balance and will help improve B12 levels too
Difference between folate and folic acid
chriskresser.com/folate-vs-...
Many Hashimoto’s patients have MTHFR gene variation and can have trouble processing folic acid.
thyroidpharmacist.com/artic...
B vitamins best taken after breakfast
Thorne Basic B or Jarrow B Right are recommended options that contains folate, but both are large capsules. (You can tip powder out if can’t swallow capsule)
IMPORTANT......If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 7 days before ALL BLOOD TESTS , as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
In week before blood test, when you stop vitamin B complex, you might want to consider taking a separate methyl folate supplement and continue with separate B12
Low B12 symptoms
b12deficiency.info/signs-an...
With serum B12 result below 500, (Or active B12 below 70) recommended to be taking a B12 supplement as well as a B Complex (to balance all the B vitamins) initially for first 2-4 months.
once your serum B12 is over 500 (or Active B12 level has reached 70), stop the B12 and just carry on with the B Complex.
B12 sublingual lozenges
amazon.co.uk/Jarrow-Methylc...
cytoplan.co.uk/shop-by-prod...
I'm just learning how important iron and diet is to thyroid function after suffering for 6 years with those terrible symptoms. I had extreme fatigue, dizziness and vertigo, finger/toe pain, hair loss, exercise intolerance, and more. After 7 weeks on Thorne iron most of these symptoms are getting better but my thyroid hormone is still low so I'm working on that but at least now I can differentiate between the symptoms of low iron and thyroid. I noticed yours is still low too.
Thank you for your reply. Until I found this group I have just trusted my GP who is lovely but now realise isn’t very on the ball with my needs. At my age you just accept it’s part of getting ancient. And when a doctor tells you that your iron levels are more than adequate but your body says they’re not. I had to be very firm to even get a copy of the blood test with them telling me that only the medically trained could fully understand the various interactions.
Same here. I realized my GP was willing to diagnose me with fibromyalgia and other autoimmune diseases but not once did he test my iron or B12 levels. He was a nice man and helped with my leave from work but he obviously missed the simple things, which turned out to be very important things. I looked over my lab tests from over the past 10 years, once I got a hold of them, and I saw so many things that were wrong. Clearly they don't understand either!
You just trust them to get it right but I suppose no doctor can be a specialist in everything. Add on all the problems with Covid increasing their pressures too. Just so grateful to this group empowering me to tackle the problems.
Hi, my symptoms and results were very VERY similar to yours. I'm in Scotland too and I went to a private haemotologist (had to go to London) who confirmed that a Ferritin level of <30 is considered severe deficiency and that my symptoms were caused by this (labs and some GPs have not yet caught up with this). It took me a while to get there as peri-meno and Hashi's made it hard to unravel everything.
You need iron badly. If a private infusion is not an option (though it's brilliant - I felt dramatically better within a couple of weeks), then take 1 Ferrous Fumarate tablet every second day - it'll take months so you have to accept that but it is easier to tolerate it and better absorbed (your body can only absorb a certain amount of iron in a 24 hour period).
You give me such hope. Thank you for replying. Rang my doctor this morning but she still cannot see anything at all amiss with my blood results but has suggested I go to see her in a week’s time. Indeed she has given me an appointment.
GPs are not always well informed about this (I have lots of close friends who are GPs and they fully admit it). It's a very under-diagnosed condition affecting (surprise surprise) many women in particular due to menstruation blood loss over time. I only know as much as I do because my OH is an Anaesthetist and they want patients undergoing major surgery to have good ferritin levels as it has an effect on recovery - they often refer for iron infusion pre-op.
Have a look at the downloads on this page as there is good information: theironclinic.com/iron-infu... think you will feel much much better if you get your ferritin up.
then take 1 Ferrous Fumarate tablet every second day - it'll take months so you have to accept that but it is easier to tolerate it and better absorbed (your body can only absorb a certain amount of iron in a 24 hour period)
That is an awfully small dose of iron to suggest for someone who is suffering from iron deficiency.
I know that there is a limit on how much iron someone can absorb at one go thanks to Hepcidin. I wrote a post about it:
healthunlocked.com/thyroidu...
However, the NHS still hasn't changed their advice on how much iron to take to treat low iron. I hope they do at some point.
I took ferrous fumarate 210mg 1 tablet, 3 times a day, starting back in 2013 (i.e. before the "every other day" research came out). It took me 21 months to raise my ferritin to mid-range because I absorb it so poorly.
Knowing what I know now, I would definitely try other options than the dose of iron I took but I am not aware of any research being done to suggest what the optimal dose for iron is with alternate day dosing if taking a therapeutic dose.
I think I would like to try ferrous gluconate 300mg (which contains 35mg iron per tablet), on the basis that adults can take up to 6 a day according to the BNF. The options for tailoring the dose according to tolerance and absorption are obviously greater with a smaller dose per tablet.
I understand, it's difficult as it seems research is ongoing and not all medics are even aware of it as yet. There have been articles about the research on alternate day dosing in Anaesthesia journals which my OH drew my attention to, and my private consultant was adamant that the limit for iron absorption per day was quite small (I forget the exact figure), and that the serum hepcidin produced, limiting further iron absorption, persists for 24 hours . He works a lot in Australia where they are much more up to date on IDWA and IDA and the corresponding treatment (they give a lot of infusions apparently!). The other problem he raised which I do definitely agree with from personal experience is that compliance in patients who are prescribed Ferrous Fumarate x3 daily is poor - largely because of gastric side effects. Therefore people often abandon it and are back to square one. I found it intolerable so the alternate day dosing would have certainly suited me better.
The only way I could tolerate the dose of ferrous fumarate 210mg I took was if I took the tablets with food. It would have slowed down my absorption of iron, but I had no choice - it was the only way I could get iron into me.
I didn't know about infusions at the time. If I had done I would probably have paid for one.