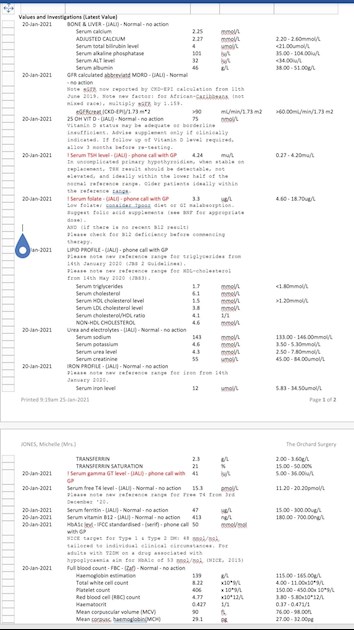
I have had a total thyroidectomy. Feeling rubbish, although looking at results not surprised, (will add the other page of results after, can only upload one on this post), as a result of these GP has increased dose from 175 levo to 200 and put me on folic acid 5mg, this is not the first time I've had folic acid, despite taking a b complex with folic acid this happens a lot. He also wanted me to start statins due to cholesterol, but after some research of my own, decided not to take them. Is there anything else that I can be doing, I'm struggling with daily living at the moment, I'm lucky to have an understanding boss! Seems I may also have a liver problem, I hardly drink alcohol, this blood test was taken 22/01, which was following Xmas and new year, when I did drink, waiting on appt for liver scan.
In need of advice on recent bloods : I have had a... - Thyroid UK
In need of advice on recent bloods
Second page of results
Which brand of levothyroxine are you currently taking Do you always get same brand
Do you take levothyroxine waking or at bedtime
Was test done as early as possible in morning before eating or drinking anything other than water and last dose levothyroxine 24 hours before test?
No other medication or supplements at same as Levothyroxine, leave at least 2 hour gap.
Some like iron, calcium, magnesium, HRT, omeprazole or vitamin D should be four hours away
(Time gap doesn't apply to Vitamin D mouth spray)
Exactly what vitamin supplements are you currently taking
Was vitamin B complex one with folate in or folic acid?
Remember to stop taking any supplements that contain biotin (most vitamin B complex) a week before ALL BLOOD TESTS as biotin can falsely affect test results
If you normally take levothyroxine at bedtime/in night ...adjust timings as follows prior to blood test
If testing Monday morning, delay Saturday evening dose levothyroxine until Sunday morning. Delay Sunday evening dose levothyroxine until after blood test on Monday morning. Take Monday evening dose levothyroxine as per normal
Thyroidectomy due to multi-nodule goitre. Aristo current brand. B complex contains folate also biotin, didn't stop before blood test, will next one. I always wait at least one hour after levo before any other meds, will now make sure at least 2 hours, I take in the morning Have used patient to patient advice from here before blood test. I also take daily dose of selenium, vitamin d with K2 and magnesium, 3000iU.
Have you ever tried strictly gluten free diet?
Many people on levothyroxine find gluten free diet helps or is essential
Ideally get coeliac blood test first while still eating high levels gluten
How do you find Aristo?
New lactose free brand, seems to suit some people
You could try taking levothyroxine at bedtime. Certainly is much more convenient.
The fact your vitamins keep dropping underlines that you’re still under medicated
But even when adequately we frequently need to supplement continuously to maintain optimal vitamin levels
But many people also need addition of T3
Thanks for the valuable information. I guess for the moment sit tight another couple of weeks for the next blood test. Then go from there. Will try to find out about coeliac test. I'll try taking levo at night, to start I'll take a half tonight and then half morning before moving to all at night. I'll need some time to read through everything you've given. My eyes are now blurry, time to sleep again.
Was thyroidectomy due to Graves’ disease or thyroid cancer
Wish I had some answer but your bloods looks exactly like mine, I’ve had total thyroid removal for graves and I’m still struggling to get all my levels right plus constantly got low iron and low calcium!
Many people after thyroidectomy can not manage on just Levothyroxine
Many people need addition of small doses of T3 prescribed alongside levothyroxine
Email Thyroid UK for list of recommend thyroid specialist endocrinologists......NHS and Private
tukadmin@thyroiduk.org
The aim of levothyroxine is to increase dose upwards in 25mcg steps until TSH is under 2
When adequately treated, TSH will often be well under one. Most important results are ALWAYS Ft3 followed by Ft4. When adequately treated Ft4 is usually in top third of range and Ft3 at least 60% through range (regardless of how low TSH is)
Extremely important to have optimal vitamin levels too as this helps reduce symptoms and improve how levothyroxine works
Dr Toft, past president of the British Thyroid Association and leading endocrinologist, states in Pulse Magazine,
"The appropriate dose of levothyroxine is that which restores euthyroidism and serum TSH to the lower part of the reference range - 0.2-0.5mU/l.
In this case, free thyroxine is likely to be in the upper part of its reference range or even slightly elevated – 18-22pmol/l.
Most patients will feel well in that circumstance.
But some need a higher dose of levothyroxine to suppress serum TSH and then the serum-free T4 concentration will be elevated at around 24-28pmol/l.
This 'exogenous subclinical hyperthyroidism' is not dangerous as long as serum T3 is unequivocally normal – that is, serum total around T3 1.7nmol/l (reference range 1.0-2.2nmol/l)."
(That’s Ft3 at 58% minimum through range)
You can obtain a copy of the articles from Thyroid UK email print it and highlight question 6 to show your doctor please email Dionne at
tukadmin@thyroiduk.org
Professor Toft recent article saying, T3 may be necessary for many especially after thyroidectomy
rcpe.ac.uk/sites/default/fi...
healthunlocked.com/thyroidu...
the best paper on this that I have seen indicates that a TSH of 0.03-0.5 is best on therapy. Above that is insufficient and below MAY or MAY NOT indicate slight overdosing
academic.oup.com/jcem/artic...
Interestingly, patients with a serum TSH below the reference range, but not suppressed (0.04–0.4 mU/liter), had no increased risk of cardiovascular disease, dysrhythmias, or fractures. It is unfortunate that we did not have access to serum free T4 concentrations in these patients to ascertain whether they were above or within the laboratory reference range. However, our data indicate that it may be safe for patients to be on a dose of T4 that results in a low serum TSH concentration, as long as it is not suppressed at less than 0.03 mU/liter. Many patients report that they prefer such T4 doses (9, 10). Figure 2 indicates that the best outcomes appear to be associated with having a TSH within the lower end of the reference range.
Prof. Tofts’ paper is one of the most interesting papers I have read. And it could explain my own issues with treatment.
Does anyone know if there was any pier review or follow up?
Also what does the following mean?
“...insufficient to maintain euthyroidism, but in whom serum T3 concentrations were in the upper part of the reference range or raised as a result of LT4 therapy.”
I thought we were aiming for T3 to be in the upper range? This appears to contradict?
Russ
You need to get your T3 levels and reverse T3 (rT3) levels checked, it's very, very important! Increasing your T4 dose may worsen hypothyroidism by increasing rT3, it did to me.
Info here:
restartmed.com/thyroid-lab-...
I was diagnosed with Graves Disease in 2003 age 56 and had RAI thyroid ablation in 2005 :
I was dosed with Levothyroxine and only ever on 100/125 T4 daily and only ever monitored on the yearly thyroid function blood test results and my dose adjusted so I came into the bottom of the TSH range, but as this made me more unwell, I was prescribed anti depressants as some sort of consolation prize.
I found this amazing forum about 5 years ago and started to read up :
I arranged a private blood test including reverse T3 and I was over range :
I see this as a normal bodily function and over range because I had been hyperthyroid.
I am now self medicating with NDT and seem relatively well on 1 + 1/2 grains which equates to just 57 T4 + 13.50 T3 - and so presume should I measure my reverse T3 now, it will have reduced substantially as my maintenance dose of T4 has virtually halved.
We all have some reverse T3 and it' a normal bodily function, but if your body is under undue strain and stresses and there have been medically diagnosed thyroid health issues, I think the whole workings can be seriously compromised, and no medic seems to know anything of any value, and we all end up trying to make sense of it all through this amazing forum and sharing experience and knowledge with people in similar situations.
Hello Jones :
Can I just add that a fully functioning working thyroid would be supporting you on a daily basis with trace elements of T1 and T2 and calcitonin plus a measure of T3 said to be at around 10 mcg plus a measure of T4 said to be at about 100 mcg :
T4 -synthetic Levothyroxine is a storage hormone that needs to be converted by your body into T3 the active hormone that the body runs on. T3 - synthetic Liothyronine - is said to be about 4 times more powerful than T4 with the average person said to need to utilise around 50 mcg T3 daily - just to function.
Your natural ability to convert the T4 into T3 can be compromised by low vitamins and minerals and its suggested that ferritin, folate, B12 and vitamin D need to be maintained at optimal levels. You may need to supplement these yourself, as you may well be in the NHS ranges, but not high enough, and optimal, for someone living without their thyroid gland.
As you will see from the above you have lost your own natural production of T3 and this actually represents around 20% of your overall well being and overtime, no matter how hard your body tries to compensate for this shortfall, you may start to feel under par.
Personally I just think if there has been a medical intervention and the thyroid surgically removed or ablated with RAI that it makes common sense to replace like with like, and that both T3 and T4 should be on the patient's prescription, for if, and probably when, they will both be needed to be prescribed to restore wellness and good health.
Some people can simply get by on T4 only : so people simply find, at some point in time, T4 doesn't work as well as it once did, and some people simply need both these vital, essential thyroid hormones need to monitored and dosed accordingly to bring them into balance.
Generally most people feel at their best when both their T3 and T4 are in the top quadrant of their ranges and balance, and at a level high enough to be acceptable to the patient.
The thyroid is the body's engine, some say, the conductor of all your bodily parts including the woodwind section, and is responsible for full body synchronisation, your physical, mental, emotional, psychological and spiritual well being, your inner central heating system and your metabolism.
I'm with Graves Disease and following RAI thyroid ablation in 2005 became very unwell in around 2014 : after over 2 years on a very unmerry NHS merry go round I had explanations except that I was low in ferritin. I found this site and stated reading, and am now so much better it simply defies my understanding of how the NHS treats thyroid related health conditions.
I can't see your blood test results too well - your TSH looks to be too high which means you are undermedicated and there is room to increase your T4 as we generally feel better when towards the top of the range. However if your vitamins and minerals are not at optimal levels this increase in T4 alone may not " do it " for you :
I can't see a T3 blood test result ? It's generally a % of your T4 result and seeing as your T4 is just around midway through it's range that in turn probably means your T3 is low and it is low T3 that causes the debilitating systems of hypothyroidism.
I am now self medicating and so much improved, and you can turn much of this round for yourself, you don't need to be a chocolate teapot !!
I had the thyroid removed 4-5 years ago, initially I felt great. Have gradually gone downhill since, the blood test before this showed as under medicated so levo went up from 150/175 on alternate days to 175 every day. These results are worse than those. I'm so fed up, also going into menopause, so that's not helping either. I may request T3 on next blood test, as I'm sure you know, NHS don't normally test it. Might also try to find and get referred to good thyroid endo, if there's one here, last endo I went to was as bad as the GP's.
Well you could take maters into your own hands and start by getting a private blood test run - companies listed on the Thyroid UK website.
When with the results and ranges post back up on here and you will get considered opinion and advise on what you can do to turn things around for yourself.
Otherwise you back at square 1 as if your doctor run the correct thyroid hormone blood panel you'll keep going around the same circle getting nowhere :
It's a massive learning curve and needs some basic knowledge and understanding but it all makes sense and you can do much for yourself.
Thyroid UK is the charity who support this amazing forum - maybe just start reading up on there and on this rolling screen as it's a bit like a jigsaw, but you will see the right bits and where they all fit together for your well being and better health.
Can I ask why you think you have liver problem? Your ALT is 32 that's not high. Mine usually 25ish but once shot up to 130 because I was using a LOT of cinnamon, I love it, in coffee, smoothie, yogurt etc it is fairly toxic to liver and within 6 weeks of no cinnamon it was back to normal. I know many very heavy drinkers whose liver enzymes don't increase so moderate drinking unlikely to be a problem. Cholesterol is often bit higher if hypothyroid mine is 0.27 over limit but under limit is considered to be worse. I won't get into station debate but I wouldn't touch them with a barge pole xx
As told by GP, assuming the gamma gt levels.
I was only looking at the liver enzymes which are all normal, iv no idea what gamma gt is but I am not a Dr xx
Have a look here:
Your doctor is not usually concerned with low or normal results, but they do tell him/her that it is unlikely that you have liver disease.
Raised GGT concentrations indicate that something is going on with your liver but not specifically what. In general, the higher the result the greater the damage to your liver. Elevated concentrations may be due to liver disease, but they may also be due to congestive heart failure, drinking alcohol, and use of many prescription and non-prescription drugs including nonsteroidal anti-inflammatory drugs (NSAIDs), lipid-lowering drugs, antibiotics, histamine blockers (used to treat excess stomach acid production), antifungal agents, anticonvulsants (seizure control medications), antidepressants, and hormones such as testosterone. Oral contraceptives (birth control pills) and clofibrate can decrease GGT concentrations.
labtestsonline.org.uk/tests...
Yes I wondered at the time if my pain killers were to blame but on reading the cinnamon jumped out at me, that was all I changed and my ALT went back to normal. I am teetotal so I knew it wasn't alcohol 😜
Thank you all for the advice and information, it is always appreciated, 7 weeks following the increase in levo, and I'm feeling an improvement, but nowhere close to well.
I have my next blood test booked for 19th March, I'll post the results, hopefully in a clearer format, as soon as I get them. Doctor has also requested T3 to be included. Liver scan to be done end of the month. I stopped taking B vitamins a week ago, so the biotin should be out of my system. Do I need to stop folic acid?