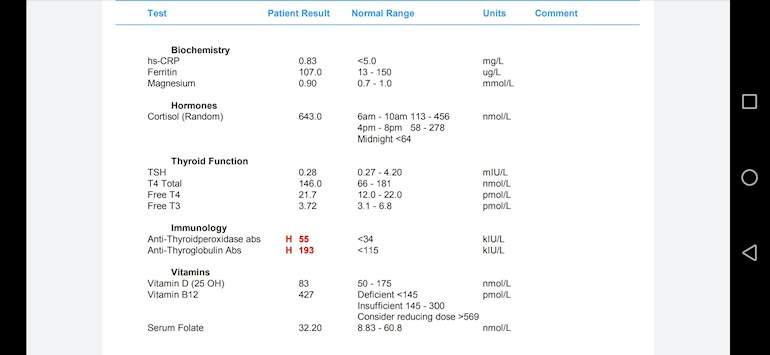
I posted my blood results (attached) on here about a week ago and I got some great advise from some very kind people regarding them. I have a telephone appt with my GP next Monday and I am worried that when I try to explain that my T3 is too low she will just say that its within the normal range and refuse to refer me to an endo. Any ideas about how to make her understand that even though it's in normal range it's still too low? Also can you only be referred to an NHS endo who is in your local health authority or can you ask to see a specific endo from a different authority? Also should I be asking her to look at my cortisol levels and if so what should I be expecting her to do? Thanks all
How to word what I need GP to do: I posted my... - Thyroid UK
How to word what I need GP to do
Be aware that any endo NHS or not can refuse to see you if they think your levels are fine enough for the gp to manage your care.
Point out that with ft4 near the top of the range if conversion was efficient Ft3 should be near the top of its range and that the Ft3 being low in comparison is causing symptoms.
That sounds reasonable to me. I'm really apprehensive about it as I have never had much success makingdoctors understand how unwell I feel and that it's because of how I am being medicated I'm sure. Thanks for your advice I shall be sure to word it in that way
You can also say that you agree that it is a range and that people's results should be somewhere in that range. However exactly where is a matter for an individual and their symptoms. And your current result is not your optimal spot. You need it higher to reflect your higher ft4.
So free T4 is 21.7 [12 - 22] = 97% through range
free T3 is 3.72 [3.1 - 6.8] = 16.75% though range
This clearly shows they are not balanced and you do not convert well.
Can you do your phone appointment on speaker phone with a MAN there to support you - ideally to emphasise that although your free T4 is so high, you still aren't as well as you were before you had thyroid trouble? Doctors often treat us as less stupid/hysterical/ill informed if there's a bloke around.
In theory you can see any endo anywhere in the country - but the GP needs to refer you and the endo needs to agree to see you. Obv needs to be reasonably convenient to get to.
It's worth doing a new post to ask if anyone near you can recommend someone. Have you had the list of T3-friendly endos from Dionne at thyroid UK - tukadmin@thyroiduk.org?
Good luck x
Thank you. I shall make a point of emphasising the difference in those percentages.
Its so sad that we have to feel such apprehension when speaking to our doctors when they should be there to help us in whatever way to make us feel well
I do have the list thank you but I would be grateful to know of any recommends in my area. I live in the Merseyside area but I would travel anywhere to be honest in order to be listened to and treated appropriately
I write an email to my surgery and attach my latest private blood results for two reasons. One, I ask them to add the test results and a copy of the email to my medical notes for future reference, but also as a running diary of my symptoms etc so there can be absolutely no misunderstandings. Two, I find it easier to document my symptoms, concerns etc so a GP (can hopefully) digest the info before my appointment. I have subsequently found that the GP's don't talk down to me any more and at least take me seriously.
Here is my latest letter (obviously I've blanked doctors names).
When I spoke to a doctor at my last annual review, they had initially suggested leaving my Levothyroxine dose at 125mcg daily rather than implement a 25mcg daily increase I had requested. Although I felt my health had improved I was still experiencing significant symptoms including debilitating tiredness, fatigue, nausea, weight gain, extreme sensitivity to the cold and cognitive symptoms including forgetfulness and difficulty concentrating. Nonetheless, at my last appointment in January, my dose was decreased by 300mcg a month due to suppressed TSH. Needless to say I still don't feel well, let alone euthroyd. Once again it has been recommended (via consultation between Dr. XXXX and an endocrinologist at XXXXX hospital) I require a dose decrease which I strongly disagree with and will not, under any circumstances agree to.
I am aware there is significant reliance on TSH levels to determine treatment and doseage, however TSH is a pituitary hormone and not an indicator of T4 to T3 conversion, T3 receptor resistance, adrenal insufficency or presence of thyroid antibodies. TSH levels can also be effected by vitamin deficiencies and insufficiencies as well as the presence of antibodies and increased inflammation. I would like to point out it is common for patients with thyroid disease to feel better, even euthroyd with a low or suppressed TSH (a study by the Society for Endocrinology in 2010 confirmed it may even be safe for patients to take slightly higher doses of thyroxine than are currently recommended).
In January 2020 my T3 (the active thyroid hormone) had only increased by 0.02 pmol/L since the previous dose increase suggesting I was (even before the dose decrease) under medicated (based on personal symptoms and research which identified T3 should be three quarters through normal lab range in order to restore function).
I am also struggling to manage my Hashimoto's Thyroiditis and note my inflammation continues to remain either at the higher end of normal lab range or slightly over. The relationship between Hashimoto's thyroiditis and key vitamins including C, ferritin, folate and B12 has been well researched. Studies have found deficencies and insufficencies are common among thyroid patients and require regular monitoring (which I do via private testing). My vitamin D, ferritin, serum and active B12 are all at the very lower end of normal lab ranges. I suspect my folate will be much the same given that it was also low when tested a year ago. I strongly suspect this, along with the presence of thyroid antibodies is causing the continued inflammation.
While I understand the reliance of lab ranges I feel the interpretation and subsequent treatment has not been uniformed. My Levothyroxine was decreased due to an abnormal result, the GP citing increased risk of heart disease due to suppressed TSH, yet my raised inflammation markers have been disregarded despite their potential health implications. With this in mind, I feel I would benefit from a more pragmatic approach to treatment. Having blood levels within 'normal' lab range is only beneficial if those levels are optimal for me. At the moment they are definitely not (based on pre-existing symptoms, antibodies and continued test results)
Given that since the Levothyroxine dose decrease my T4 and T3 have (predictably) dropped significantly, I request you consider once again increasing my Levothyroxine to 125mcg daily in an attempt to raise my T4 and T3. I also request you consider whether my low serum and active B12 levels require further investigation as I'm sure you are aware, patients with autoimmune thyroid disorder have a high prevalence of B12 deficiency, particularly pernicous anemia. I also ask you to consider if I would benefit from a loading dose of B12 which will enable me to self supplement a maintenance dose to retain optimal levels. I have already doubled the dose of my vitamin D supplement from the recommended 10ug daily (as per a previous GP appointment) and fully implement a gluten free diet in an attempt to control Hashimoto's symptoms and antibodies. By addressing all these issues I believe I will begin to reduce the level of inflammation, optimise my treatment, normalise and stablise my TSH.
I should also add in my email 'intro' I also requested evidence of increased risks due to suppressed TSH and queried how an associated risk can possibly be an indication of being over medicated.