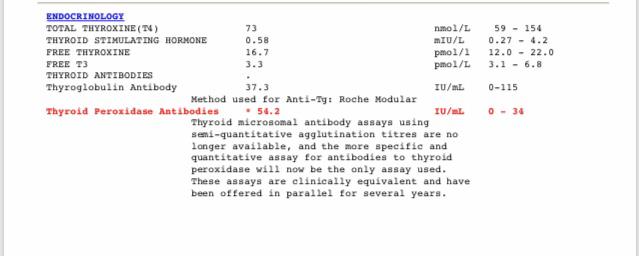
I have Graves and I’m on 2.5mg Carbi a day. Just had some Blue Horizon bloods showing rock bottom FT3, this puts me in chronic fatigue / post exertional fatigue territory from a symptom point of view. I’m not seeing my Endo for another month and he’s redoing these bloods before my appointment, plus TRAb. I would really like to push for add back therapy, i.e. adding a little Levo or similar to my Carbi to boost levels. I don’t want to stop Carbi if my TRAb is still positive. Has anyone had success getting an Endo to agree to this? My last Endo, who I’ve recently left, point blank refused to consider it, choosing to focus on my TSH instead. I think these bloods show the folly of relying on TSH in a Graves patient. The other thing I could do is half my dose again to 1.25mg. Anyone have any thoughts? Thank you.
Anyone on add-back therapy for Graves? - Thyroid UK
Anyone on add-back therapy for Graves?
I have been on block and replace for 3 years. It was the treatment recommended by my endo as on Carb alone I was becoming HypoT. My Trab is still high at 16 and so I have a high chance of relapse and intend staying on this for a while. We did want to achieve lowest possible dose to minimise possible side effects. This took a lot of monitoring which is why I think many docs avoid it. We finally settled on 10 mg Carb. Plus 50mcg. Levo. and I now feel great. All my bloods are now within range which seems to keep the docs happy.
TSH is suppressed?
Before starting B and R I had reduced Carb. From 20 to 5mg. TSH was still supressed. On BR my TSH slowly increased to within range. This made my Endo very happy !
Wow that's pretty amazing to hear
: ) congratulations! Almost all readings are in range : )
Read some time ago, a post on the forum, the poster said her endo did not like it that her TSH was still suppressed. I cannot remember the context. When she asked him why, he said he was worried this put her at risk of having a stroke or cardiovascular problems. That really stuck in my mind
That poster could possibly have been me ! Most endos want TSH in range. After lots of reading I decided risk was minimal as long as it was below range but not fully supressed. If I find the paper that helped me reach this conclusion I will post link.
Do you mean block and replace treatment ? I had it and it wasn't successful, very difficult to get the doses right.
Not classic block and replace, which tends to have a higher dose of carbi for a complete block. It’s more you’re on a very low dose of carbi and still going hypo, so you “add back” Levo whilst keeping the carbi low.
As you have PA as well it's important to regularly retest vitamins
Do you supplement a good quality daily vitamin B complex ?
When were folate, ferritin and Vitamin D last tested?
Supplementing a good quality daily vitamin B complex, one with folate in not folic acid may be beneficial.
chriskresser.com/folate-vs-...
B vitamins best taken in the morning after breakfast
Recommended brands on here are Igennus Super B complex. (Often only need one tablet per day, not two. Certainly only start with one tablet per day after breakfast. Retesting levels in 6-8 weeks ).
Or Jarrow B-right is popular choice, but is large capsule
If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 7 days before any blood tests, as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
Are you on strictly gluten free diet?
If not ...
While still eating high gluten diet ask GP for coeliac blood test first or buy test online for under £20, just to rule it out first
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
I’ve got all that covered, thanks. I self inject alt day hydroxo and take adenosyl subs, take all cofactors, and do better on FA than MF. I’ve been GF / DF for many years although negative for coeliac. My new Endo also has me on a low carb diet, sugar/fruit free for now, to address insulin resistance. Other problems we’re addressing are histamine intolerance, oestrogen dominance, slightly wacky adrenals, gut healing protocol. He’s put me on iron as my ferritin / saturation wasn’t ideal. So there’s a lot going on that could be impacting my numbers. Ironically I feel better now than at the beginning of the year, but still that low FT3 prevents me from taking that next step and being able to do things like exercise or just things that are extra to the normal rhythm of my day.
Surely an interesting topic
Hi Coconutty, not sure if this is any use to you, I've not read through it myself. Came across the article while looking for other info.
Adding carbimazole to levothyroxine increases triiodothyronine and improves outcome in patients with primary hypothyroidism: a preliminary study from Egypt