We keep seeing claims that the top of the TSH range in the USA is 3.00. (And that “they” start treatment if TSH goes above that.) This has been repeated by people who really, really should know better such as professionals. As well as ordinary people like us.  We all have to base our understanding on what we see and find for ourselves.
We all have to base our understanding on what we see and find for ourselves.
The other day I posted some links on this post:
healthunlocked.com/thyroidu...
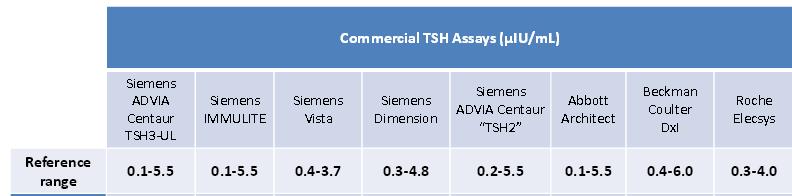
- and one of them contained a list of TSH ranges from real, live USA labs:
Reference range
0.1 - 5.5
0.1 - 5.5
0.4 - 3.7
0.3 - 4.8
0.2 - 5.5
0.1 - 5.5
0.4 - 6.0
0.3 - 4.0
The PDF is linked here:
aacc.org/members/loc_sectio...
And the above appears on page 30.
As you can see, the very lowest top of range is 3.7. I guess that the ranges vary by the precise analyser/kit in use more than any other single factor.
This claim of 3.00 being the top of the reference range has been repeated all over the place. But, so far as I can tell, it is not backed up by what I have seen. PR4NOW posted about this the other day - seems it was a recommendation but was never implemented.
Further, the very papers which made the recommendation of tightening the ranges did not adequately take into account the differences between the various analyser machine/kit manufacturers and labs. All too many papers seem to assume standardised reference ranges (at least across the country the paper comes from) but this is simply sloppy science/medicine. They vary within every country which has more than one make of TSH analyser in use.
Rod
Image is a small fragment of the quoted PDF showing the various analysers used and the reference ranges for each of them.
 ) that the earlier TSH tests were prone to interference by, for example, macro-TSH. Hence a higher top of range.
) that the earlier TSH tests were prone to interference by, for example, macro-TSH. Hence a higher top of range.