Just posting because I am pleased to see research, new studies, and updated guidelines (related to GCA and/or PMR) being conducted, discussed and released!
Apparently, there will be new recommendations presented that will offer guidelines, "...for everything from diagnostic tests such as serology, imaging and biopsy, to remission induction and maintenance therapies, to managing refractory disease, to possible surgery."
healio.com/rheumatology/vas...
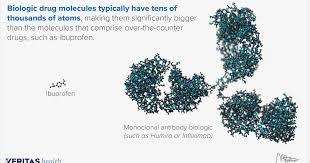
*{A biologic drug (biologics) is a product that is produced from living organisms or contain components of living organisms. Biologic drugs include a wide variety of products derived from human, animal, or microorganisms by using biotechnology.}