A long term study looked at molecular response (MR) vs progression for PV and ET. It was for Rux therapy, although it's possible these molecular correlations apply to IFN too. Of interest is the 12+ year study length and easy to read comparison of MR to progression.
I have a newly acquired interest in Rux so will be sharing my experiences and findings.
--
Some notes:
-One pt with MPL got Complete MR (CMR, undetectable VAF) )on Rux. This is news since I think MPL does not respond well to IFN (comments welcome)
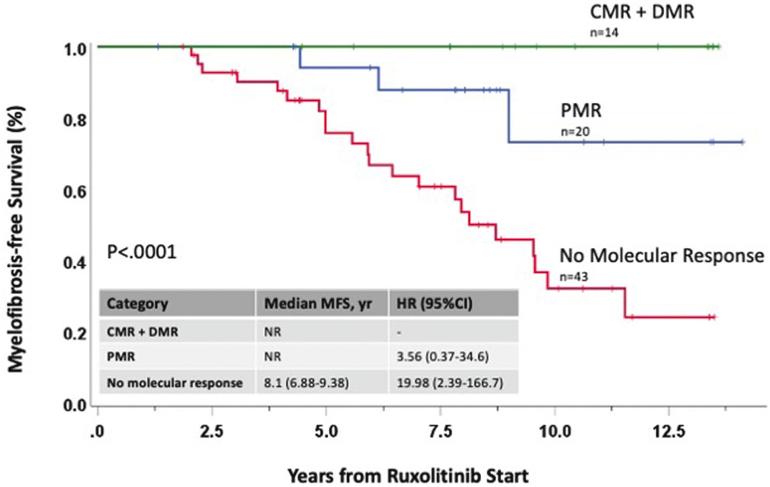
-MR makes a big difference in progression.
-Lower starting VAF (mutation burden) gives better MR.
- "All 3 pts who transformed to AML had not obtained any molecular response."
-The plot here is easy to read, green line is all who got to less than 2% VAF. Zero progression over 12 years. This is consistent with 2% limit being important with IFN. Blue got VAF cut by at least half and retains a large progression benefit.
--
- A starting VAF (mutation burden) of less than 60% led to much greater likelihood of MR.
-Compared to pts with decrease to <2% VAF, having no response led to 19X more likely to progress, and partial MR was ~4X more likely.
-Undetectable (CMR) was in 6.5% of pts. This compares well with IFN I believe.
-Tracking MR while on Rux, (or IFN) is a good idea
-It's possible combo IFN+Rux could improve MR for some (my opinion, it's not addressed here)
--
My Dr insists Rux is very good therapy. I'm looking more into why.
--