This has been covered in some form before. But I came across this report that summarizes misc info from Cornell in a nice clean manner. See link, it's easy reading.
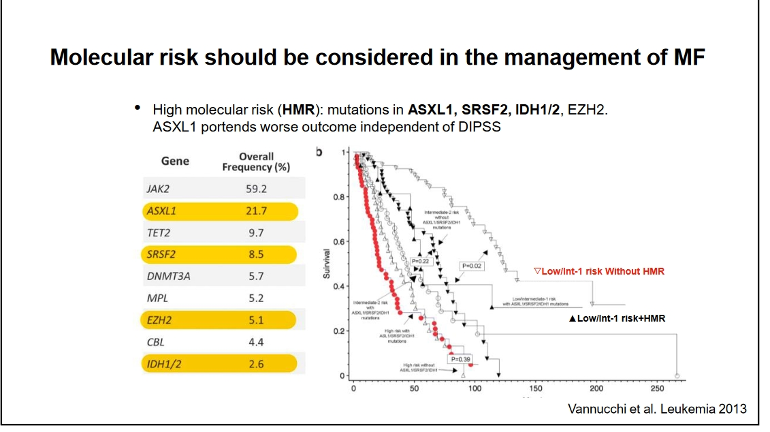
A specific takeaway is with the high risk (HMR) mutations in yellow here they lean toward SCT (stem cell transplant) if possible rather than waiting. See #1 guidelines below. There's also a good plot, slide #30 in the report, of the survival benefits of SCT vs various risk levels.
-Note that TET2 and DNMT3A are not in the high risk category with MF. But high risk ASXL1 is most common non-Jak2 in MF (22%).
For MF they recommend INF for lower risk earlier MF, at low doses, see 2nd set of guidelines below. Low doses is different from the current PV practice we see, maybe because of over reductions of some blood counts with INF+ MF.
--
For PV most info is familiar, but buried on slide #20 is a note that Phlb increases risk of fibrosis. I don't recall this anywhere else, but it may be in the long term INF Cornell reports we've discussed.
--
There's also this statement <<First step towards optimal treatment is making an accurate diagnosis
Bone marrow histology is crucial!>> This has not been so clear in our posts and experience.
--
Another chart shows there are 1763 MPN trials registered now. We like that. USA has the most ongoing, 1200, (one supposed benefit of our outrageous drug prices) Euro is next at 429.
==
#1- Risk-adapted treatment guidelines for myelofibrosis:
• Low to intermediate-1 risk (by IPSS/DIPSS/DIPSS-plus score)
- Observation alone for asymptomatic patients
- First line HU for symptomatic splenomegaly
- Ruxolitinib for highly symptomatic splenomegaly or constitutional symptoms
- consider Interferon (rIFNα)
• Intermediate-2 to High risk (by IPSS/DIPSS/DIPSS-plus score)
- Allogeneic stem cell transplant (SCT) for eligible patients
- First line Ruxolitinib for splenomegaly
==
#2- INF for MF:
What about Interferon in Myelofibrosis?
WCM experience:
- IFN should be used at low doses for sufficient duration (>12mo).
- Patients who are most likely to benefit are those with:
low-grade (grade 1-2) BM fibrosis,
No massive splenomegaly (<10cm on exam),
lower DIPPS score (low-int 1),
absence of high molecular risk mutations.