I came across this interview including Dr. Gotlib, Stanford MPN expert. It's regarding MDM Inhibitors for HU resistant/intolerant PV, MF
"Experts Explain MDM2 Inhibition and Clinical Trial for MPN Patients"
patientpower.info/myeloprol...
--
It includes this statement from him:
<<we know that patients with hydroxy resistance or intolerance have about a six-fold increased risk of death and a seven-fold increased risk of transformation to myelofibrosis>>
I've heard that a good HU response is broadly positive prognostic but never heard such an extreme effect.
Are any Members familiar with more data on this? Maybe related to non-driver mutations?
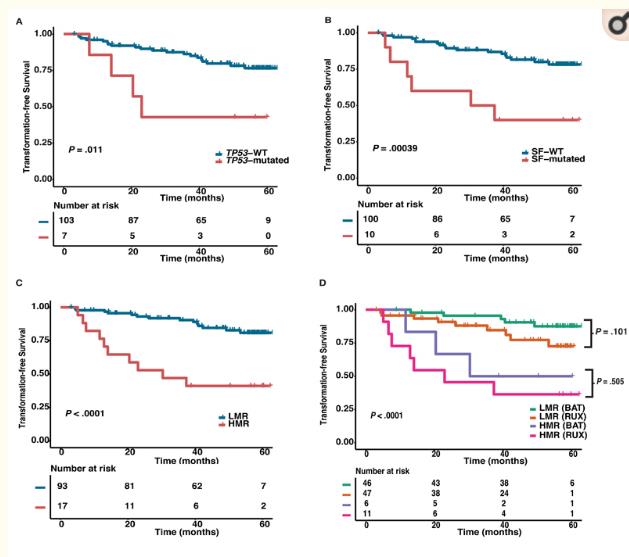
This article is related to the subject and implicates TP53 and SF-- mutations:
ncbi.nlm.nih.gov/pmc/articl...
<<We found a particularly high prevalence of TP53 and splicing factor mutations, which was strongly predictive of subsequent disease transformation, and was not mitigated by RUX>>
In the image LMR=low molecular risk (without SF or TP53 mutations) My NGS sequencing looked for these. Another good reason to know your NGS results.
So Rux didn't help but MDM inhibitors could be useful here. No study of INF in this set.