I sent this to skyshark based on some info he posted but I was hoping for the whole group to chime in.
I had 3 rounds of FCR in 2018 stopped because of profound neutropenia.
I relapsed exactly 2 years later and though I did not start Tx until the 5 year point in 2023, would have gladly started it 9 months ealier due to B symptoms.
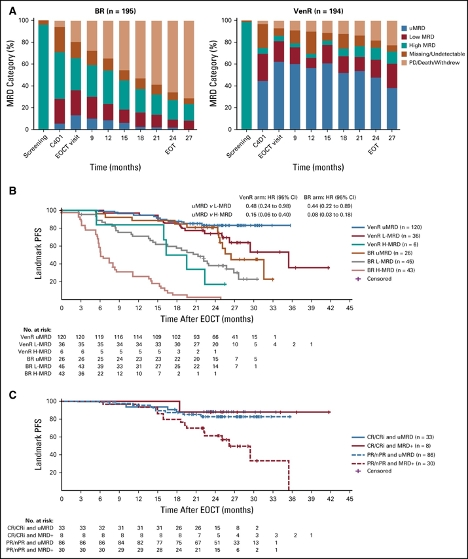
I've been curious about improvement of uMRD status with longer duration of Ven after completing the V + O cycles. I am at 14 months with intolerable side effects that greatly impact my quality of life. At 13 months I was uMRD 4 in PB and had 4/10,000 CLL cells in Marrow.
My oncologist showed me some data from Murano III for R/R patients on V + R that showed not much better MRD status was achieved after the first 9-12 months compared to those at 2 years total on Ven. And said I could stop V now if I wanted and just see what happened.
However, in the same Murano study group, stopping treatment early led to shorter PFS where as dose reduction did not. I had a har
I had a hard time following the logic of either of these 2 studies.
Skyshark you have the citation for your comment
"CLL14 by end of cycle 6, 72% were uMRD-4, 61% uMRD-5. By cycle 12 that number had hardly changed but uMRD6 had increased from 34% to 50%. Dr Brian Koffman's (n=1) observation is that a factor of 10 reduction gives nearly an extra year before next treatment."
Just hate to stick it out another year on Ven if my MRD status is not going to improve much and I end on some sort of treatment for the same amount of time now v. later
DO ANY OF YOU HAVE ANY OTHER DATA OR intepreatation of these studies to guide my decisions about how long to put up with the Ven. Eg does 10 month longer only buy me 10 months less overall treatment over a life span?
Thx
Skipro