Anyone diagnosed with atherosclerosis/heart disease, who has had a heart attack, stroke, a bypass or a stent, or indeed anyone who has had any kind of heart problem due to plaque in their arteries, will surely have asked themselves this question.
We're told by the NHS and the BHF that we can't remove plaque from our arteries, but what about new plaque? Are our medication and life style choices preventing new plaque being formed, or are our arteries getting worse over time?
I've always thought that, apart from some serious investigative work like an angiogram, we'll never know the answer.
But some remarkable research gives us a tool that, even though it's far from the complete answer, at least gets us a bit closer to addressing that question. And what's more it uses an often ignored part of the blood test that most of us already have from the annual cardio check-up with our GP's.
If you dig out your blood test you'll find a score for HbA1c, or Haemoglobin A1c. It will be a number, such as 29 mmol/mol, or 48 mmol/mol. It's a measure of how much glucose (sugar) has stuck to our red blood cells. It's a useful measure because it doesn't require us to have fasted before the blood test, indeed it's really an average showing how our bodies have processed the sugar and carbs that we've eaten over the previous few months.
If that number is 42 or above your GP may warn you that you're pre-diabetic, and if that number is over 48 your doctor may refer you to an NHS Diabetes Prevention programme, or perhaps prescribe some additional medication.
But if that number is below 42 the most likely thing is that your GP will just ignore it.
I recently came across a very large piece of high quality research that basically asks, is there a relationship between our HbA1c scores and the amount of plaque being formed in our arteries?
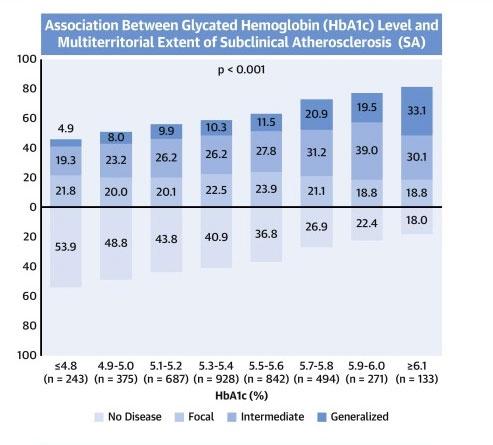
And the answer is a resounding yes. As the graph at the beginning of this post shows, the higher our HbA1c scores then the more plaque is being formed.
Couple of things that may help you understand this graph.
Firstly, there are different ways of stating HbA1c scores, this research uses % scores instead of the mmol/mol scores. But they're easy to translate, for example the very low 4.8% in the above graph is equal to 29mmol/mol, and the very high 6.1% is equal to 43mmol/mol. You can translate your score from mmol/mol to % using the following tool, so you can exactly where you personally fit on this graph,
hba1cnet.com/hba1c-calculator/
The second thing to understand is that the research draws a distinction between no plaque (disease) at all, finding an isolated example of plaque, and finding lots of plaque in multiple locations across different arteries. That's the meaning of the "no disease, focal, intermediate, generalised" scores.
What we can clearly see is that the higher our HbA1c scores then the more likely that new plaque is being formed in our arteries.
But unless our HbA1c scores are 42 or over our doctors are unlikely to discuss this with us. And that's a shame as there are plenty of things, from life style to medication, that most of us can do to bring our HbA1c scores down. I've gone from low 40's to low 30's with weight loss, exercise, and a healthier diet, and what's more I've kept it there for nearly five years. But armed with this research I'm asking myself if I can't go further, maybe I can tweak my diet, weight and exercise regime a bit more and see if I can get back to HbA1c scores in the high 20's?
The research concludes that HbA1c scores are so significant they should be added to the statistical tools that our GP's use to predict our risk of heart attacks and strokes. Furthermore the research says that GP's should discuss with their patients, at much lower HbA1c scores, that if they make different life style choices or possibly consider medication such as metformin, then they can probably reduce their HbA1c scores and in doing so reduce their risks of angina, heart attacks, and strokes.
That all makes perfect sense to me, but I guess with our overworked NHS it's down to us to educate ourselves and change our life styles without waiting for a prod from our GP's.
If you want to read the original research in full you can download the pdf here,
sciencedirect.com/science/a...
Finally, thanks to aaq91, who recently pointed me towards a video from a heart doctor which linked to this research.