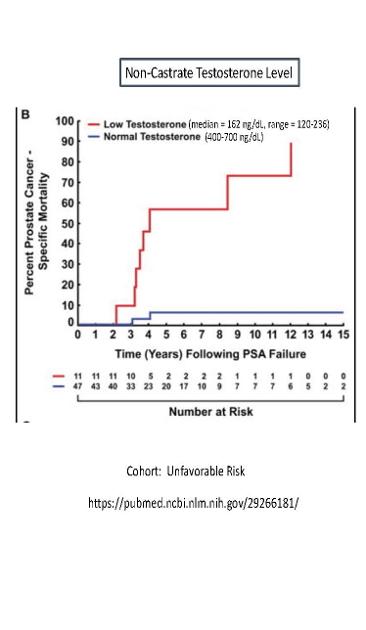
Here's a plot from Atkins (2018) that shows the Percent risk of Prostate Cancer-specific Mortality versus time following a first PSA failure, for two different non-castrate testosterone levels (Low-T and Normal-T). The low testosterone levels are: median = 162, range = 120-236 ng/dL. Normal T is 400-700 ng/dL.
The Cohort is "Unfavorable Risk", according to the paper.
The plot shows that having normal T levels are protective, when compared to "Low" testosterone levels (120-236 ng/dL).
At 5 years after first PSA failure, the prostate specific mortality rate is about 7% for normal T, versus 58% for "Low" T. That's a huge difference, which only gets larger with longer time.
The paper also reports that the PSA doubling time is 2.8 months for Low-T and 10.6 months for Normal-T. Also, the median survival time is 4.1 years for Low-T versus 7.6 years for Normal-T. These are significant differences!
These results suggest that doing TRT after a first PSA rise might be very effective at prolonging life.
The paper doesn't mention this, but it would be interesting to find out if this Cohort was castration-resistant or not. Likely, they are, because the "Low-T" levels are non-castrate levels.