My cancer seems pretty aggressive. Whenever it starts to rise slowly after one treatment or another, 6 months later PSA starts rising quicker. I'd love to try Lute177 but lack the funds. Are there clinical trials available in the US?
Went castrate resistant after a year ... - Advanced Prostate...
Went castrate resistant after a year of Orgovyx --now PSA still climbing after 30 days of Zytiga. PSMA scan shows two spine mets. Now what?
I am sorry to hear about your situation. It did scare me since we both have very similar situations. Just curious as to why you calculate the total psa, does it have any significance?did you talk to your MO about this? Best of luck in finding the right treatment
oh, by the way, what is your T level now? As you know, you are only castrate resistant if your T level is low and psa rising. This is the only definition I know of.
Here are all the clinical trials in the US:
prostatecancer.news/2020/08...
Thanks. I looked at those but frankly I don't know which apply to me. I have two small tumors as indicated on a recent PSMA scan, as of five months ago, one-year of Orgovxy has begun to fail. And one-month ago started Zytiga which also has failed.
If you failed Zytiga and never had chemo, these apply:
clinicaltrials.gov/ct2/show...
clinicaltrials.gov/ct2/show...
Thanks again. I'm not sure what a randomized trial is. Does that mean one group gets a placebo and the other gets Lutetium? So there is no way to tell if you got the Lutetium?
It might help you if you actually read the links I provided.
"Participants will be randomized on a 2:1 basis to receive Lu177-PSMA (Investigational Arm) or standard of care hormone therapy (Control Arm). The Control Arm will consist of treatment with either abiraterone with prednisone or enzalutamide depending on the clinical judgement of the investigator. Participants who are randomized to the control arm who demonstrate radiographic progression [within 34 weeks] may be eligible to crossover to receive Lu177-PSMA."
It is not blinded - you will know when you are getting the radiopharmaceutical.
The other clinical trial is not randomized. Everyone gets 67Cu-SAR-bisPSMA
Clinical trials are the only way you can get a PSMA-targeted radiopharmaceutical in the US without getting chemo first.
thank you for that explanation. I do indeed read all of those links and material several times. I just don’t understand it.
Thanks for saying that. I've seen so many of these that it doesn't occur to me that others might not understand. I will break it down phrase by phrase:
"Participants will be randomized on a 2:1 basis to receive Lu177-PSMA (Investigational Arm) or standard of care hormone therapy (Control Arm)." They will sign up 400 patients in total. When patients sign up, they will randomly assign 267 of them to get Lu177-PSMA, which is call the "investigational" group; and 133 patients to get Xtandi or Zytiga, which is called the "control" group.
"The Control Arm will consist of treatment with either abiraterone with prednisone or enzalutamide depending on the clinical judgement of the investigator." In your case, you would get enzalutamide (Xtandi) if you are assigned to the control group, because you've already failed abiraterone.
"Participants who are randomized to the control arm who demonstrate radiographic progression [within 34 weeks] may be eligible to crossover to receive Lu177-PSMA." All patients are monitored with bone scans and CTs. If you are in the control group, and you show new or larger tumors within 34 weeks, you will be invited to get Lu177-PSMA. This is called "crossover." If you are in the investigational group and you show new or larger tumors within 34 weeks, you will be offered some other therapy (e.g., docetaxel). Either way, they will continue to closely monitor you for 156 weeks (3 years).
The other trial has no control group - everyone gets differing amounts of the investigational drug.
I hope that is more clear. At any rate, the investigator is required to fully explain the trial and its risks before you sign up.
We all greatly appreciate your knowledge and efforts on this forum, TA. We may quibble about this and that here and there, but I suspect we all read all or most of your input and respect it--even if we don't always express that.
Thank you again. The concern I have now is the potential damage to other tissues with such a low volume disease like mine. It’s my understanding that if the LU 177 does not have enough cancer to attach to the it attaches to healthy tissue and can actually invade the bones into the marrow. I would assume that doctors have an adjusted dosage for low volume disease. What do you think?
It's a legitimate concern. Bone marrow isn't the problem for you because the PSMA ligand won't go there if there is no PSMA-avid PCa there. But it does go to the salivary glands and the kidneys. However, note that they are not using Pluvicto in either trial. Pluvicto is 177Lu (the radioactive part of the molecule) attached to a ligand called PSMA-617. The ligand is the part of the molecule that attaches to the PSMA on the cancer cell surface. The new ligands they are trying out hopefully have more affinity for prostate cancer cells and less affinity for salivary and tear glands. Also, some are not excreted through the kidneys. They are using the experimental ligands PSMA I&T in the one trial and SAR-bisPSMA in the other. Part of what they are doing is monitoring toxicity in patients.
In the 67Cu-SAR-bisPSMA trial, they are starting patients at a very low dose, and increasing it. They hope to find a dose that is less toxic but still effective. 67Cu is a beta emitter with slightly higher energy (it kills more cancer cells) than 177Lu, but a much shorter half-life (it delivers its energy faster). And each molecule has 2 PSMA ligands - twice as likely to attach to a PSMA molecule on the cancer cell. There is a new source for 67Cu, so it may not have the availability problems that have recently plagued 177Lu.
They test for the amount of PSMA-avid tumor tissue you have with the new ligands too. Hopefully, 68Ga-PSMA-I&T will detect more of your cancer than 68Ga-PSMA-11 (which, along with Pylarify, is currently used). And, in the other trial, they are using 64Cu-SAR-bisPSMA, which hopefully will be more sensitive.
Thanks again for the education. What makes PSMA I&T safer than LU177? I'm going to try for this trial.
It would help you understand if you did not call it Lu177. Lu177 is only the radioactive part of the molecule. It is used in other radiopharmaceuticals that have nothing to do with prostate cancer (e.g. Lutathera). Now re-read my reply keeping that in mind.
Thanks again for your patience. What about combining the 68Ga-PSMA-I&T with SBRT and Provenge? If that is possible what would be the sequence of those treatments?
68Ga-PSMA-I&T is an experimental radioindicator for a PET scan, not a treatment. Did you mean - what treatments can you have after 177Lu-PSMA-I&T ? If so, docetaxel, Xofigo, and Provenge are all possible. But that is in the future and there may be more possibilities. SBRT is used for painful bone metastases.
Why is chemotherapy not considered in your situation? Can you consider SBRT of your mets if it is feasible? Could you find a competent MO?
UCLA Dr. Kishan wants to do SBRT on the two small tumors and thinks that might kill whatever is castrate resistant. I guess the only way to know for sure is to try and see if my PSA decreases while still on Orgovyx.
Just don't do low volume toxic lutetium before concidering chemotherapy at your low PSA.
I wish your plan works for you.
Can you find rather sooner than later a competent MO if you don't already have one?
What you are doing is masking the PSA. I understand that. I am doing the same. My last PSA was 0.51 after radiating my prostate. I did radiation instead of chemo or enzalutamide. I had a CRPC only visible in my prostate.
Without that radiation my PSA would be above 2 by now. We will see how it will go.
We hope that I can stay on Degarelix alone.
I didn't want to do chemotherapy if I can get rid of the visible cancer with high precision SBRT radiation.
My MO for sure would not recommend systemic radiation at this point. You have to think about the toxicity.
I didn't want to start enzalutamide at this point. I afraid breading out some nasty strains like neuroendocrine PC.
Take care.
so do you guys think there’s more side effects to Pluvicto or chemo?
It is not about which one is toxic. Bought of them are toxic.
It is about that at your low volume cancer pluvicto would end up mainly in your body and not in your cancer.
The more tumor load one has it will take more ligand into the tumor and there will be less ligands for other tissues. The inverse may be true and that is the reason that some places do not take patients who are oligometastatic for Lu 177 PSMA treatment because they are concern with damaging the kidneys.
tango65GeorgeGlass:
I consulted with 3 MOs and 2 ROs, My case was presented to the tumor meeting at the local cancer center,. All these people advised to do SBRT if oligometastatic even when having mCRPC.Dr Eiber at the Technical University of Munich, refused to do Lu 177 PSMA because there were only 2 mets."
Uptake of PSMA-ligands in normal tissues is dependent on tumor load in patients with prostate cancerFlorian C. Gaertner, Khalil Halabi, [...], and Markus Essler
Lu 177 PSMA is as good as other therapies for MCRPC which usually control the cancer for 3 or 4 months longer than SOC .. The same happens with chemo, Xofigo, Provenge etc.
I believe Lu 177 PSMA treatment is more effective when used early.
All the cancer therapies do not work well when used in patients with very large tumor load and with multitude of treatments. Unfortunately most of the clinical trials are done in this type of patients.
Why is it so that the liquid biopsy yield with better results when the PSA is above 10 and bone metastatic?
The liquid biopsy works if enough cfDNA/RNA and circulating cells are collected in the blood sample.
It seems is related to the tumor load. There was a study some years ago showing that in people with few bone mets and PSA below 10, blood the samples did not had enough cell free DNA/RNA and or circulating tumor cells to do the genetic and IHC studies.
there is a recent article indicating that a least a PSA of 5 is needed to have a good yield in a liquid biopsy along with higher ALP (bone metastases) and other variables.
Is both a PSMA scan and a FDG scan needed to check heterogeneity of Prostate Cancer for LU-177 (Pluvicto) treatment in the US?
No, it is not needed.
The Hofman’s group in Australia started to use it in a randomized control trial to select patients who will benefit more from Lu 177 PSMA treatment. For example, if a FDG PET/CT showed tumors which were PSMA negative those tumors will not be treated by Lu 177 PSMA treatments and those patients were not admitted to the trial.
Other criteria to select patients had been used in trials such as mets with SUV values similar to the liver or at least one met with a SUV of 20 or more. These criteria eliminated all patients which did not have metastases with those values.
More recent they are concentrating the selection of patients using the whole body mean SUV value (do no ask me how they can calculate this value) and based in this value decide which patients will benefit from Lu 177 PSMA treatment.
If one has a cancer with low PSMA expression (mets SUVs less than the liver) , a FDG PET/CT may be useful to make a final decision about treatment with Lu 177 PSMA, since there may be mets which are not seen in the PSMA PET/CT and appear in the FDG PET CT.
Other criterium which could eliminate patients for Lu 177 PSMA treatment is diffuse bone marrow infiltration in a PSMA PET/CT.
If these patients are treated with Lu 177 PSMA, many normal blood cells in the bone marrow could be affected by the radioactivity of the Lu 177 PSMA attached to cancer cells in the proximity and make the hematological problems even worse.
The bone marrow of these patients could be affected less if they are treated with Ac 225 PSMA since the radioactivity of alpha particles travels less distance than the beta particles of the Lu 177.
SV Viking,
Kishan can probably hit the spine mets in only 3 treatments of SABR/SBRT. Your PSA may, or probably will drop down again quickly.
I had 3 days of SABR to my T5 last January and my PSA is lower one year later. It is painless. Felt like I had lifted something too heavy at gym for a week, then went away. I would get on this sooner than later. No fear, no pain. Just do it. Get insurance pre appvl and get it done. Remain on your ADT throughout. Best of luck, Mike
Some centers perform SBRT off ADT so as to see the effectiveness of the radiation on PSA. If PSA is suppressed by ADT, you don't know how effective it was.
My RO is fine that I am on ADT , but my cancer is CRPC. He said that ADT is good for radiation as it makes the cancer more sensitive to radiation. He would not be happy if I would use Abiraterone plus Prednisone for example as he would like to save that for the future as everything fails one day.
The more tumor load one has it will take more ligand into the tumor and there will be less ligands for other tissues. The inverse may be true and that is the reason that some places do not take patients who are oligometastatic for Lu 177 PSMA treatment because they are concern with damaging the kidneys.
I wish that you are cured before lutetium becomes useful for you in extending your life for 4 months.
I hope that you also look into other options for you. You are rationalizing why is it good to continue on your path.
I understand you.
Still why would not consult Dana Farber cancer institute or some other centers of excellence with a question to give you an opinion about the possibility of the cure. Just to see and learn what they will say. I know that you are focused on your way. I wish you luck but cancer always finds it's work around even the best treatment.
TA said that BAT does not extend life expectancy. I understand that you are focused on the quality of life now.
Still try to build up knowledge about (even only theoretical) possibility of the cure.
We all should hope in that. Even I am hoping.
No
I understand your situation.
I really tried to make it clear that we all should hope for the cure. I was explicitly told by my ex wife that I should expect to be cured. I don't want you to change curse. I just wish that you are a bit more open minded about other options even if you don't have to change curs. It is up to you. This is only my opinion. After high level thinking.
You don't have to change curse just inform yourself from the best institutions. I am much behind you in everything still I believe we all should keep an open mind. Better if you just inform yourself.
I don't know, maybe for me it is easier to remember Dana Farber. I just know that people are really very positive about the team in Dana Farber. For me a good team is the most important. Maybe has to do about Jung teaching.
I believe John Hopkins is not paying enough their people. MSKcc is probably also very good. Contact any of them if you want. Sorry about my ignorance about your book. These things always changing. Difficult to keep up. I also have sleep apnea and that makes my life even more difficult. I wish you all the best and good luck.
I began my PC journey 3 years ago with a prostatectomy at MSKCC. Over the past 6 months dealing with a recurrence, I am of the opinion that MSKCC is a surgical hospital and that's where it ends. I actually did some research and sought out one particular RO for my new treatment. I do stay with MSKCC for my ADT, however, they are merely writing my scripts, as the advice and direction they offer is useless to me as it contradicts what I have been told by Mayo, Johns Hopkins and RWJ.
Prostateless, I personally had great Radiation success with Dr Sean McBride at MSKCC. 5 treatments of SABR MSK Precise to my prostate, and 3 treatments to T5. They are World Famous for more than just surgery.
1 year later Pylarify PSMA PET shows mo PCa in prostate, no PCa in any bones or organs. Yes to 3 lymph nodes that have shown on every scan since Dx. Trying to get those removed or radiated now.
Mike
Medications aside, I would consider a radical diet change (for myself). I would cut out all sugar and ask my MD to help monitor during some rigorous periodic fasting. It is not for everyone but the health benefits are many.
We always have new developments. That is why it is a good idea from time to time contact the best and the brightest.
You can continue your plan just don't miss the opportunity. I also believe that you are not curable, but who I am? I went to the RO to find out the latest development in radiation therapy. The know more than us.
Everything usually fails with the cancer.
Still my ex wife believes in that the cure is coming, just hang around long enough (that is her thinking) and recommendations.
Again you just stay informed and keep alive by always receiving the best possible medical advice.
There are centers outside the USA that offer a combination of LU177 +/-AC225 and SBRT. I know this is possible in both Australia and Turkey. There is also a trial of this combination in the USA listed at the clinical trials web site. clinicaltrials.gov/ct2/show...
Maybe for him the best would be just to do SBRT or if not feasible than as Mateo beach recommended above. But I am not an MO. The more aggressive treatment with 177 lutetium and 225AC should be saved for later.
I don't know the right answer and I am not sure anyone really does. But in theory the SBRT or other external beam radiation would address the macroscopic disease seen at the level of detection by PSMA PET/CT and the radioligand would address the microscopic disease below the level of detection by imaging limitations.
Only if it is PSMA positive and even then only the PSMA positive cancer and would live alive the PSMA negative cancer. And even then it would not totally eradicate the PSMA positive cancer as even the same cancer can be more and less PSMA positive, therefore surviving the treatment.
Nobody died from micromets.
The problem is even if you eradicate the PSMS positive cancer the PSMA negative cancer could slowly take over the free living space and as a result of that you can't use anymore with great confidence the PSMA PET scan to follow up your cancer if the PSMA negative cancer takes over (repopulate).
That would be my worry.
Don't underestimate my ex. She is way more intelligent than me.
I am divorced and I don't drink alcohol, only coffee as I have sever form of sleep apnea.
🤦♂️😂😂
wouldn’t hurt to stop zytega start nubequa. It might work since an atiandrogen might block any T. That orgovyx doesn’t suppress. Worth a try if you haven’t already. Good luck
I'd make sure the testosterone is below 50, below 20 is best. Then looking at the PSA can be done monthly or even every 3 months. If it gets up over 2, then I would talk about the next step. If androgen-based treatments fail quickly, chemotherapy is generally preferable. Of course LU-177 is also an option although you might have to do chemo first.
My testosterone is <10
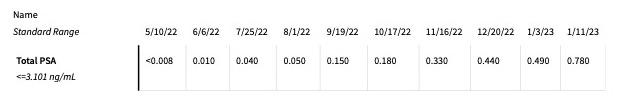
PSA seems to be rising pretty quick.
Yes, but the numbers are still small. You don't look at doubling time with PSAs that low. And you are checking your PSA almost every week which just creates more Prostate Specific Anxiety IMO. When did you start Zytiga?
Started Zytiga 30 days ago
I wouldn't call it a failure until your PSA goes up above 2 and doubles from there. Also would want to see imaging if there is progression.
If Zytiga fails in the next month or two, I would talk to your doctor about chemotherapy. You only have to commit to doing one cycle at a time.
You are doing fine and you are in capable hands of an RO. Who is your MO? Does he have a say?
MO is Dr Dorf