Good Morning All,
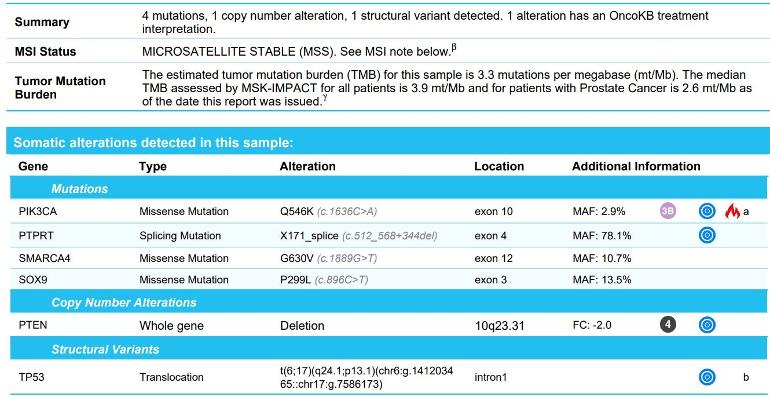
If anyone on here has knowledge they could share on the attached pathology which calls out some mutations, that would help me to understand where I sit, and maybe more so, what I can do about it. When asking my Medical Oncologist to review it, he basically tells me there is no action we can take towards it. If there is a person who understands these, and can maybe share some of your experience on what I could bring up during my next visit, that would be great. I understand that no one on this site can give me medical advice, I am merely looking for a better explanation on what I have on the report, and what what I can potentially do to address them, if anything. I have had an RARP on 8/11/22, (all scans were clear prior to the surgery) Post Surgery Pathology showed, all Margins Clear, 15 lymph nodes clear, but Focal EPE was present. Gleason 4+3, with some Tertiary pattern 5. PSA 7 weeks out was a detectable .20, then .27, then .28. To complicate things, I have Crohn's, so a complete salvage radiation attempt has it's risks. We did a PSMA 11/18 to see if we see anything. There was very very slight uptake in 1 obturator lymph node, of which my doctors don't feel is compelling enough to target it with focal radiation. They are suggesting to sit tight a bit, and monitor the PSA, and when I get to .5, rescan. If I am going to wait, I want to know if I can do anything with the mutations I've attached. Thanks for taking the time to review my post.