hi all,
I’m really desperate for some advice and support. I have posted a couple of times before and I’m waiting for my endo appnt in April.
- had several years of unexplained fatigue & flu like symptoms which would come and go. Subsequently given diagnosis of fibro
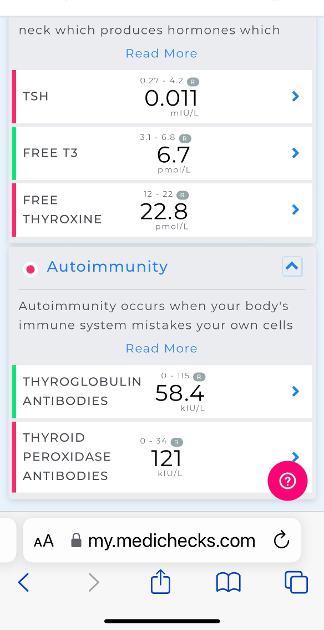
- last year after 3 bouts of covid within 6 months; took a medichecks thyroid panel which revealed elevated TPO
- several bloodtests over the past year have looked ok but my TSH is in the low end of normal
- recent stomach issues led to bloodtests which revealed TSH of 0.03 and FT3 just over and FT4 within top end of range
- prescribed Carbimazole by doc within suspected hyper / graves (but I know this cannot be diagnosed without appropriate testing). I decided to not take Carbimazole at first thinking this diagnosis most likely incorrect and current state could be transient
- my thoughts were similar to other replies I’d received that this could be Hashis and it could be a transient hyper phase
- symptoms worsened by way of severe mental health deterioration. panic attacks, feeling like going to die. I thought level may be getting worse so decide to try carbi.
- in the following 6-7 days on carbi, a loss of appetite, severe nausea, a complete deterioration of mental symptoms, feeling so anxious, crawling out of my skin. Calls to 111, my GP, thoughts of feeling like I’m going to die. Started to suffer with severe hypnic jerks all night when trying to sleep, as soon as I closed my eyes and breathing started to slow - a feeling of adrenaline rush, tingling in arms, heart pounding. 2 days of no sleep whatsoever Woken out of my sleep so violently one night, I ended up calling 111 who sent an ambulance at 4am. By the time they arrived I had calmed a little.
- stopped carbi immediately. Not if it was a bad reaction causing me to feel so bad. Did a medichecks test again which gave results as attached - TSH has dropped but others are just out of or within range. Went to docs who has pretty written this all off as anxiety but this feels so different to any I have felt before. ECG normal & blood tests repeated. I haven’t had results yet but was told by reception that they are back and they look similar to previous.
- heart rate is slightly elevated, especially today.
I have also had mild intermittent pain in the thyroid area
My apologies if any of this post is inappropriate or needs to be taken down. I am just absolutely desperate for some support of advice. I feel like I shouldn’t be feeling this bad if my levels are not wildly out range?
I feel hopeless and depressed, as well as extremely anxious. The only thing calming me down is diazepam (which have never ever taken before).
Any words of comfort or advice would be most appreciated