I can see from my medical records that I'm being set up for the prognosis of 'hysterical woman'
To set the scene
As previously described, I've had a lot of symptoms since mid 2021 with no resolution and the only positive anti-body test is for Tpo. I have lots of physical symptoms from an enlarged goitre, low potassium (medicated), pulsatile tinnatus (although no GP has tested to check if it's objective or subjective), high blood pressure, raynaud's syndrome, sliding haitus hernia, bile in stomach, enlarged gallbladder, and now haemorrhoids).
I also have a lot of subjective symptoms - aches and pains in hands and feet, temperature control issues - too hot and too cold.
Most blood tests are in range, though not all.
A CT scan done because a gastroendoscopy showed a extrinsic mass pushing into my stomach, showed an enlarged gallbladder (but no stones or slurry) and a small amount of fluid around my heart. I am having a ultrasound to investigate further. I have had several episodes of heart palpitations in the past (usually a mild fluttering but once for 20 mins) which seems to coincide with my potassium falling.
When my blood pressure was checked in Aug an average of 138/92 was deemed acceptable and I continued with 5mg ramipril daily. My notes state I was told I would have my blood pressure taken in a years time unless I had vision problems, head aches or dizziness, in which case I was to go back to the GP. I was not told this in person at all - I read this on my notes which are now online. I don't really care how this information was conveyed though it makes me wonder how often GPs are covering their arses by pretending to say things that weren't said in the notes.
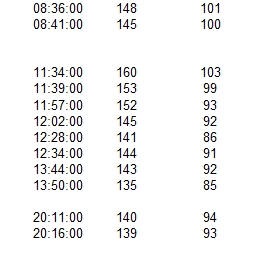
Mid September I started to get mild headaches which disappeared when I got up. This slowly worsened to having a mild headache until mid afternoon. Sometimes painful enough to need tablets and sometimes not. I didn't want to make an appointment with the GP on these vague symptoms so I started taking my BP and found it would rise until mid afternoon and then fall back. I've attached a sample day so you can see what I mean. Some days it rose above 180/100 but then fell back to around 140/90
Anyway because of the high bp readings and because of the pain in my chest (which was more like something stuck in my chest than a pain - like swallowing something very dry and needing water to help it go down) I was sent to A&E. I didn't want to go as the chest pain felt exactly like I'd had previously with palpitations which had already been looked at).
When at the hospital I was asked if it could be anxiety - I mean, sure it could be but why would the results go up and down in such a regular pattern if it was anxiety? I was then asked if I felt anxious about my blood pressure going up. I said no, but when it was over 150 systolic I did feel a bit anticipatory - like something was going to happen, like Christmas or going into an exam - so not necessarily a good thing or a bad thing, just something. I also said that feeling disappeared when the blood pressure went down again.
TL;dr
I've just checked my GP notes and the A&E said I was taking my blood pressure loads of times in a day and getting an anticipatory feeling from it. No mention of any headaches of course. So should I leave it? Or write to the surgery and at least put forward my recollection? It feels no win, I do nothing and it's there on my notes and I do something and it reinforces I'm an anxious patient.