I have been well for the last 9 yrs or so and now started to feel unwell..
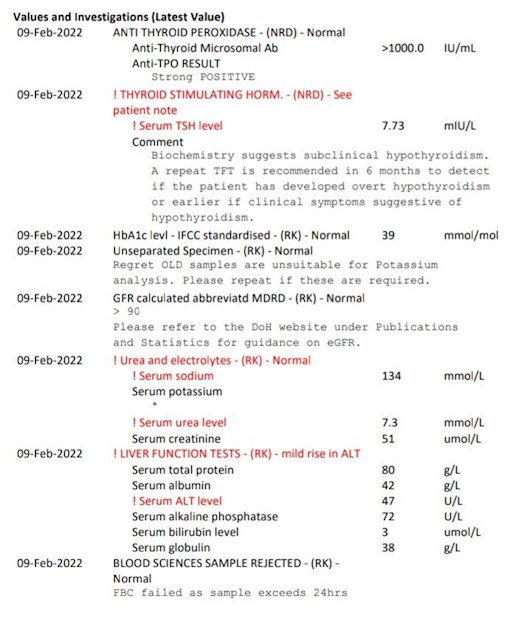
Here are my blood results, Dr just wants to test again in 6 months..
Thoughts and advice pls..
Ty..x
I have been well for the last 9 yrs or so and now started to feel unwell..
Here are my blood results, Dr just wants to test again in 6 months..
Thoughts and advice pls..
Ty..x
When we've been diagnosed and take thyroid hormone replacements, the aim is to bring TSH to around1 or lower with Free T4 and Free T3 in the upper part of the ranges.
Your TSH is rising, so I believe you need an increase in your dose.
I'm not on any medication, my Dr doesn't think it's needed yet..I will call tomorrow to insist on it.I'm feeling really crap..
Doctors have been told not to diagnose a patient with hypothyroidism until the TSH reaches 10. I think more emphasis should be put upon the clinical symptoms the person may have developed.
Was your blood draw at the very earliest, and fasting (you can drink water) and if you had already been diagnosed and taking thyroid hormones, you take them after the blood test - not before.
With TSH over 5 and high thyroid antibodies you should have bloods retested in 6 weeks (not 6 months)
Assuming second test shows TSH over 5 you should be prescribed levothyroxine
Standard starter dose of levothyroxine is 50mcg
Bloods should be retested 6-8 weeks after each dose increase (or brand change in levothyroxine)
It will take 6-12 months to slowly increase dose levothyroxine up until adequately treated
See flow chart on top of page 2 here
gp-update.co.uk/Latest-Upda...
Have you had coeliac blood test done yet
Coeliac should be tested for at diagnosis of autoimmune thyroid disease
Essential to regularly retest vitamin D, folate, ferritin and B12 too
When were these last tested
What vitamin supplements are you currently taking
I haven't had them tested for yrs, just started taking vit d...Have not been tested for coeliac..Should my Dr test that or is it private testing?
Assuming you aren’t already on strictly gluten free diet?
Yes high thyroid antibodies confirms autoimmune thyroid disease
nice.org.uk/guidance/ng20/c...
1.1.1 Offer serological testing for coeliac disease to:
people with any of the following:
persistent unexplained abdominal or gastrointestinal symptoms
faltering growth
prolonged fatigue
unexpected weight loss
severe or persistent mouth ulcers
unexplained iron, vitamin B12 or folate deficiency
type 1 diabetes, at diagnosis
autoimmune thyroid disease, at diagnosis
irritable bowel syndrome (in adults)
first‑degree relatives of people with coeliac disease.
pubmed.ncbi.nlm.nih.gov/286...
Vitamin D deficiency is frequent in Hashimoto's thyroiditis and treatment of patients with this condition with Vitamin D may slow down the course of development of hypothyroidism and also decrease cardiovascular risks in these patients. Vitamin D measurement and replacement may be critical in these patients.
pubmed.ncbi.nlm.nih.gov/273...
Vitamin D insufficiency was associated with AITD and HT, especially overt hypothyroidism. Low serum vitamin D levels were independently associated with high serum TSH levels.
pubmed.ncbi.nlm.nih.gov/300...
The thyroid hormone status would play a role in the maintenance of vitamin D sufficiency, and its immunomodulatory role would influence the presence of autoimmune thyroid disease. The positive correlation between free T4 and vitamin D concentrations suggests that adequate levothyroxine replacement in HT would be an essential factor in maintaining vitamin D at sufficient levels.
ncbi.nlm.nih.gov/pmc/articl...
Our results indicated that patients with hypothyroidism suffered from hypovitaminosis D with hypocalcaemia that is significantly associated with the degree and severity of the hypothyroidism. That encourages the advisability of vit D supplementation and recommends the screening for Vitamin D deficiency and serum calcium levels for all hypothyroid patients.
Same applies to low B12 - extremely common in hypothyroid patients
All patients who are hypothyroid should have B12 tested
ncbi.nlm.nih.gov/pubmed/186...
There is a high (approx 40%) prevalence of B12 deficiency in hypothyroid patients. Traditional symptoms are not a good guide to determining presence of B12 deficiency. Screening for vitamin B12 levels should be undertaken in all hypothyroid patients, irrespective of their thyroid antibody status. Replacement of B12 leads to improvement in symptoms,
ncbi.nlm.nih.gov/pubmed/169...
Patients with AITD have a high prevalence of B12 deficiency and particularly of pernicious anemia. The evaluation of B12 deficiency can be simplified by measuring fasting serum gastrin and, if elevated, referring the patient for gastroscopy.
Folate supplements can help lower homocysteine
ncbi.nlm.nih.gov/pmc/articl...
Levothyroxine can decrease serum homocysteine level partly; still its combination with folic acid empowers the effect. Combination therapy declines serum homocysteine level more successfully.
Low ferritin frequent in hypothyroidism